Ovarian Cancer
Integrative
Care
Guidelines
Examples
Integrative
Therapies
Treatment
Terrain
Wellness
Risk
Integrative
Programs
Commentary
More
Information
Quick Reference GuideOpen a 2-page quick reference summary of the therapies best supported by evidence for use with ovarian cancer: |
Our goal is to help you live as well as you can for as long as you can using an optimal integrative combination of conventional and complementary therapies and approaches.
Key Points
|
Many women with ovarian cancer are interested in going beyond conventional cancer therapies—that is, having an integrative approach to care that blends the best of conventional and complementary therapies. Your reading this indicates that you are likely one of these women.
Perhaps you have just been diagnosed with ovarian cancer or with a recurrence of your cancer. Now you may be embarking on surgery, chemotherapy, radiation therapy or some combination of these—maybe even all three. You are curious to see if complementary therapies or healing practices could help your treatment be more effective or bolster your resilience or prevent or manage treatment side effects.
Or maybe you’ve completed your treatments and you want to know what else you can do to keep the cancer from coming back or keep it at bay. Perhaps living with ovarian cancer has brought on difficult emotions, or made it hard to sleep well or challenged your relationships. Is there help for that?
Or perhaps you’re dealing with advanced cancer and your conventional treatment options are slim—you ask "Are there any complementary therapies that would help me?” Or perhaps you feel you have limited time to live, and you want to bring the best quality to your life, however long that is.
So, what can I start with now? Any of the 7 Healing Practices are a good beginning in creating a body that cancer doesn’t like. These practices support you through and possibly enhance your treatment. Ultimately, let your intuition guide you in choosing where to start with these healing practices. The 7 Healing Practices lead off the Integrative Therapies section of this handbook.
We have scoured the research literature to find what natural products (such as curcumin) and off-label drugs (such as metformin) might be beneficial or harmful in dealing with ovarian cancer. We have also found novel approaches such as chronomodulated treatment—scheduling your chemotherapy to coincide with your body’s optimum circadian rhythms for killing cancer cells and protecting normal cells.
Optimally and safely using natural products, off-label drugs and unique administration methods happens best under the care of licensed healthcare providers who are knowledgeable and skilled in integrative cancer care. We help you explore these therapies in depth, as well as find help in putting together the options best for you.
Laura Pole
Integrative Care in Ovarian Cancer
Authors
|
No matter where you are in your experience with ovarian cancer, there’s good reason to seek integrative care: Women with ovarian cancer who followed a weekly individualized integrative medicine program during chemotherapy or palliative care had improved quality of life. They saw improvements in appetite, general well-being and ability to complete their conventional treatments. They also noted better control of symptoms such as fatigue, pain, anxiety, sleep disruption, nausea and cognitive impairment (see at right).1
Our goal is to help you live as well as you can for as long as you can using an optimal integrative combination of conventional and complementary therapies and approaches. Before investigating integrative care in ovarian cancer, we recommend reviewing integrative cancer care in general. For cancer care to be considered truly integrative, patients and their cancer treatment teams work together to find the best blend of conventional and complementary therapies that have been shown to be effective and safe.
We also recommend that you learn about your body terrain, which is your internal environment that is influenced by external factors such as the foods you eat, the chemicals around you, and the light and radiation you’re exposed to. It’s also influenced by internal factors such as stress hormones, sex hormones, your fitness level, your feelings of being loved, and your sense of purpose. This body terrain can influence the tumor microenvironment—the biochemical and physical interaction of cancer cancers and normal cells—in which the cancer exists, making it either more or less likely to spread. You can sometimes improve your body terrain with integrative practices. See Body Terrain and the Tumor Microenvironment.
Symptoms of Ovarian Cancer
|
Clinical Practice Guidelines
- National Comprehensive Cancer Network:
- Professional Guidelines (Login required)
- Guidelines for Patients: Ovarian Cancer
- American Society of Clinical Oncology: Gynecologic Cancer
Examples: Treatment Approaches from Noted Specialists and Researchers
Bastyr Integrative Oncology Care—A Naturopathic Oncology Approach
Naturopathic oncology care is complementary rather than alternative to conventional care—complementary therapies are used in conjunction with conventional treatments. Naturopathic oncologists are oriented to deliver integrative oncology care in tandem with their conventional oncology colleagues. For more information, see our discussion of naturopathic medicine and oncology at Integrative Medical Systems in Practice in the US and Canada.
BCCT advisor Leanna Standish, ND, is a fellow of the American Board of Naturopathic Oncology (FABNO) and works within the research institute of Bastyr University. Dr. Standish has been leading research studies investigating integrative therapies provided by naturopathic oncologists, as well as the costs and outcomes of that care.
A 2013 news article2 described preliminary results from the Bastyr University Integrative Oncology Research Center (BIORC) in treating 12 patients with stage 4 ovarian cancer. In looking at preventing recurrence, the researchers found that with their protocols, 83 percent of patients were still alive at three years. This is substantially higher than the 49 percent survival reported in the Surveillance, Epidemiology, and End Results Program (SEER) national data for those receiving conventional standard care (for all stages). Bear in mind, however, 12 patients is a small number—too small to conclude that these results are significant in comparison with the large SEER database.3
BIORC includes intravenous (IV) therapies. Of 46 patients, 18 received IV therapy, including IV artemisinin. At three years, a treatment effect was becoming apparent.
Bastyr University is also involved in the Canadian/US Integrative Oncology Study (CUSIOS): Advanced Integrative Oncology Treatment for Patients with Advanced Stage Cancer: A Prospective Outcomes Study, which is recruiting patients until January 2021.
Natural Products Used in the BIORC Stage 4 Ovarian Cancer Protocol
According to Neil McKinney’s Integrative Naturopathic Oncology4
- Intravenous (IV) ascorbic acid
- Turkey tail mushroom (Trametes versicolor)
- Curcumin
- Bromelain
- Quercetin
- ECGC
- Helixor M mistletoe (made from apple tree mistletoe)
Integrative Oncology Program, The Oncology Service, Lin and Carmel Medical Centers, Clalit Health Services Israel
Patient Expectations in Using Complementary ApproachesOne study found that patients using complementary medicine expected their gynecologic oncologist to be actively involved in the process of integration within supportive care and that complementary medicine consultations would focus on improving well-being.5 |
Lin and Carmel Medical Centers Haifa and Western Galilee District of Israel has an integrative oncology program. One of their leading services is integrative gynecologic oncology, based on a very close collaboration with their gynecologic oncologists. The integrative gynecologic oncology program is co-directed by Professors Eran Ben-Arye and Ofer Lavie.
According to Dr. Eran Ben-Arye, patients are referred by their gynecologic oncologists to the Integrative Oncology Program, where they begin by consulting with an integrative physician who develops a patient-specific complementary integrative medicine plan. The referring gynecologic oncologist is expected to contribute to the plan and support the patient in following it. Typical complementary therapy services:6
- Guidance on using herbs and dietary supplements
- Acupuncture and other manual-movement and body-based methods, such as acupressure, reflexology, qigong, the Paula and Feldenkrais methods
- Mind-body-spirit therapies, such as guided imagery, music therapy and spiritual care
- Anthroposophic medicine
The Integrative Oncology Program conducts research to explore the effectiveness of the patient-centered integrative model as a whole rather than a specific modality or intervention. Their studies focus on improvement in quality of life as well as improved adherence to chemotherapy protocols, mostly carboplatin and taxol.
Main findings:
- Greater chemotherapy completion: Participating in and adhering to a patient-oriented complementary integrative medicine treatment program may be linked to completion of the planned chemotherapy regimen, as shown by a higher relative dose intensity (RDI), especially with carboplatin and paclitaxel.7
- Reduced drug use: The intervention may lower the need for drugs for managing symptoms, especially non-opioid pain relievers and anti-anxiety drugs.8
- Reduced fatigue: The intervention was associated with reduced cancer-related fatigue and improved other outcomes related to quality of life, especially among those who adhered to the regimen by having four or more treatments within 30 days of each session.9
- Reduced gastrointestinal symptoms: Breast and gynecological cancer patients experienced improved appetite, nausea/vomiting, mouth sores and/or pain, heartburn, abdominal flatulence and/or pain, and diarrhea or constipation. Greater benefit was seen in patients attending at least four treatment sessions.10 A separate study found reduced gastrointestinaI concerns, with fewer chemotherapy-related hospitalizations. Including consultation with a registered dietician during complementary integrative medicine treatments led to greater reduction in nausea.11
- Improved quality of life: Improvements were seen in fatigue, physical function, role functioning, pain, drowsiness, anxiety, sleep disruption and other outcomes related to quality of life. Greater benefit was seen in patients attending at least four treatment sessions.12
- Altered patient perspective: Patients’ experiencing empathy, emotional support, togetherness, and being treated as an individual seemed to generate internal processes and helped patients feel they weren’t alone in their struggle. Patients felt a sense of agency, actively participating in the healing process.13
In sum, this program finds that patient-tailored complementary integrative medicine interventions may improve quality of life and well-being of patients undergoing chemotherapy and palliative care. These benefits come through both specific and non-specific mechanisms.14
Integrative Programs, Protocols and Medical Systems
|
For more information about protocols and programs, see our Integrative Protocols and Programs page. |
- Plans, protocols, and programs
- Alschuler & Gazella complementary approaches15
- Bastyr University Integrative Oncology Research Center (BIORC) protocol
- Block program16
- McKinney protocols17
- Traditional systems
- Ayurveda
- Traditional Chinese medicine18
- Traditional Korean medicine19
Integrative Therapies in Ovarian Cancer
The Ultimate Guide to Cancer: DIY ResearchThis guide from Ralph Moss, PhD, BCCT advisor and leading chronicler of integrative cancer treatments, shows you how to use four of the main tools that doctors use to decide on the best cancer treatments. It will help you learn why some cancer treatments that look good in clinical trials may not work for “real world” patients. It will help you answer two questions that the doctor may be hesitant to answer in the detail you need to decide about treatment:
|
7 Healing Practices: The Foundation

Let your intuition guide you in choosing where to start with these healing practices.
Any of the 7 Healing Practices are a good beginning. Eating well and moving more pack a powerful one-two punch in potentially improving treatment outcomes, enhancing quality of life and/or reducing risk of recurrence in ovarian cancer. Moreover, evidence shows that managing stress, sleeping well, creating a healing environment, sharing love and support and exploring what matters now can help women with ovarian cancer. Ultimately, let your intuition guide you in choosing where to start with these healing practices.
Eating Well
We at BCCT believe that eating well is one of the therapies that may help enhance your cancer treatments as well as restore your health, improve your quality of life and reduce your risk of recurrence. However, we emphasize that eating well alone will not likely prevent, cure or control cancer. Like every other therapy or approach included on this website, eating well is one component of an individualized integrative plan rather than a stand-alone therapy.
Treating the Cancer
The impact of diet on ovarian cancer survival:20
| Higher Survival | Lower Survival |
|---|---|
|
|
The researchers also found no association between total vitamin C, vitamin E, beta-carotene and retinol from diet plus supplements and ovarian cancer survival.21
Medline Plus recommends changes such as these to improve your poly- to monounsaturated fat ratio:22
- Snack on nuts instead of crackers or cookies
- Choose fish over red meat
- Add freshly ground flaxseed to foods
- Replace butter or margarine with healthier oils such as olive oil
Reducing Risk
Food choices are associated with ovarian cancer risk, although sometimes studies find conflicting results:23
| Lower Risk | Higher Risk |
|---|---|
|
|
- No reduced risk of recurrence was found from double-brewed green tea as a maintenance intervention in women with advanced stage ovarian cancer after standard treatment.24
- Some studies have reported an increased risk with a pro-inflammatory diet (high levels of saturated fatty acids, trans fatty acids and cholesterol),25 but two large, prospective cohort studies did not find an association.26
No significant associations are reported for red meat, eggs, fruit, vitamin D, vitamin C, coffee or four major carotenoids (alpha-carotene, beta-cryptoxanthin, lycopene and lutein). Lycopene (sources include tomatoes and other red vegetables and fruits) shows inconsistent results, but with more advantage among premenopausal women.27 See a recommendation for eating eggs in the Commentary section below.
Reduced risk was found for “an Asian diet”, but details of the diet were not reported.28
Optimizing Your Terrain
Foods can impact terrain factors to either promote or deter cancer growth and spread:
- Foods with a high glycemic index quickly raise blood sugar and may lead to chronic hyperinsulinaemia (abnormally high levels of insulin in blood), which is a potential risk factor for cancer.29
- High levels of triglyceride and low levels of HDL (high density lipoprotein, a type of cholesterol) correlate with a high severity (stage 3 or 4) of epithelial ovarian cancer.30
Moving More
Our Moving More summary has ideas on weaving this healing practice into your integrative cancer care plan.
Treating the Cancer
- Low muscle density at diagnosis and loss of muscle mass during treatment may be associated with worse survival outcomes.31
- Vigorous physical activity may benefit survival32
Managing Side Effects and Promoting Wellness
Benefits:
- Higher physical well-being for ovarian cancer patients engaging in increased moderate to strenuous physical activity during chemotherapy33
- Decreases in behavioral fatigue, cognitive fatigue and symptoms of depression, and improvements in sleep duration, sleep problems and daytime dysfunction for women who recently had surgery and completed their first cycle of adjuvant chemotherapy34
- Posttraumatic growth (positive psychological change experienced as a result of adversity and other challenges) in gynecological cancer survivors35
- Quality of life improvements in ovarian cancer survivors in a 2015 review of non-randomized studies;36 however, no effect on overall quality of life or specific aspects of quality of life (physical, emotional, social well-being and fatigue) in gynecologic cancer survivors in a 2018 review and meta-analysis37
Reducing Risk
- Risk reduction among the most active women in case–control studies but inconsistent results in cohort studies38
Managing Stress
Living with ovarian cancer can be stressful, and unmanaged stress can be harmful. Managing your responses to stressful situations and stimuli is possible and can benefit your health in many ways. Several complementary approaches promote healthy responses to stress: natural products, mind-body approaches, eating well, sleeping well and sharing love and support. See Managing Stress to explore taming stress and aiming it in a helpful direction.
Managing Side Effects and Promoting Wellness
- Improvements in quality of life and psychological flexibility as well as reduced distress, emotional disturbances, physical pain, and traumatic responses in patients receiving Acceptance and Commitment Therapy (ACT)39
Reducing Risk
- A large longitudinal study found that women with high posttraumatic stress disorder (PTSD) symptoms had a two-fold greater risk of ovarian cancer compared to women with no trauma exposure.40
Optimizing Your Terrain
- Chronic behavioral stress results in higher levels of stress hormones in tissues, greater tumor burden, and a more invasive pattern of ovarian cancer growth in mice. Tumors in stressed animals have increased formation of blood vessels (angiogenesis) and other markers of disease progression.41
Sleeping Well
Sleeping well can have profound ripple effects: reducing risk for ovarian cancer, managing stress, improving mood and energy, and modulating your immune system, to name a few.
Some lifestyle behaviors can promote quality sleep. For example, going to bed before midnight is associated with longer sleep in ovarian cancer survivors in the first six months following treatment.42 Explore this vital healing practice in BCCT’s Sleeping Well summary.
Reducing Risk
- Compared to average sleepers (7-9 hours per night), long sleepers (10 or more hours per night) had an increased risk of estrogen-mediated cancers, including ovarian cancer.43
Creating a Healing Environment
If you are trying to reduce your risk of cancer recurrence, or if you are at risk for ovarian cancer, creating a healing environment may be an important part of your wellness plan. Ideas for reducing harmful exposures linked to ovarian cancer and increasing your exposure to clean air and water, nature and beneficial light are reviewed in Creating a Healing Environment.
Reducing Risk
Many environmental exposures are associated with increased risk of ovarian cancer. Reducing or eliminating these exposures in your life can reduce your risk:
- Talcum powder used in the genital area, with varying risk according to cancer subtype44
- Endocrine-disrupting chemicals (EDCs) can cause cell growth in estrogen-responsive ovarian cancer cells.45 Hundreds or even thousands of EDCs are used in consumer products, including foods and food packaging. Those with known or suspected impacts on ovarian cancer cells include these:
- Bisphenol A (BPA)
- Hormone residues in meat, poultry and dairy products
- Some pesticides, such as organophosphates
- Asbestos46
- Ionizing radiation, such as x-rays47
Sharing Love and Support
The experience of being surrounded by love, family and friends who care about you, and the kindness of strangers—including doctors and other healers who care for you—is for many a powerful experience. Sharing Love and Support guides you in this practice to light the path to your healing.
Managing Side Effects and Promoting Wellness
- Social support predicted lower psychological distress and higher psychological well-being among women with ovarian cancer.48
- Social support was associated with improved mental state and various aspects of quality of life in women with ovarian cancer undergoing chemotherapy.49
- Compared to those who felt alone, helpless and emotionally distraught, women with ovarian cancer who felt loved and supported and who kept up their morale had more combative natural killer (NK) cells—lymphocytes identified for their ability to kill tumor cells.50
Reducing Risk
- A Swedish study found a decreased risk of serous ovarian cancer in women with fewer people available for informal socializing.51 This is opposite to findings (above) that greater social support is associated with better disease outcomes after diagnosis. The authors speculate that perhaps informal socializing in a large social network may “imply stressful expectations to support others to a higher degree.” Because this is the only study we could find with this result, we await further research to confirm and explain these results.
Exploring What Matters Now
Whether you approach meaning from a spiritual or religious perspective or from a practical perspective, paying attention to what matters to you now is perhaps one of the best places to start in making decisions about your care. This exploration may also improve your response to treatment, lower your distress and improve the quality of your life. Look inside BCCT’s Exploring What Matters Now summary.
Treating the Cancer
Greater decline in levels of CA-125 (a biomarker of ovarian cancer) during treatment were associated with higher levels of optimism at the start of chemotherapy.52
Managing Side Effects and Promoting Wellness
Lower levels of distress and a positive association with health-related quality of life in epithelial ovarian cancer patients undergoing chemotherapy were seen with higher levels of optimism.53
Chemosensitivity TestingIn many ways, each case of cancer is unique. Your personal body terrain and tumor microenvironment, which is a combination of genes, nutritional status, stress response, circadian rhythms, fitness, microbiome, history of infectious disease, hormone levels and much more, is as unique to you as your fingerprints are. Your body and tumor may not respond exactly like others to any given treatment. If feasible, your healthcare team can collect a live sample of tumor tissue and send it for chemosensitivity testing to identify your cancer’s responses to both standard and complementary therapies. Test results can identify which chemotherapies and natural products are likely to be either most effective or ineffective or in treating the tumor. Medical advocate and BCCT advisor Gwen Stritter, MD, writes, “Ovarian cancer is one of the few cancers I know of where oncologists will do chemosensitivity testing right after initial diagnosis.” Indeed, the National Comprehensive Cancer Network (NCCN) guideline for ovarian cancer says that a number of their member institutions use chemotherapy/resistance and other biomarker tests to help select chemotherapy when multiple chemotherapy options are available. However, the National Comprehensive Cancer Network (NCCN) states that the current level of evidence of using this testing is not strong, and they do not recommend such testing. The American Society of Clinical Oncology (ASCO) advises that this testing not be used in ovarian cancer except in the clinical trial setting.54 If your doctor is following the NCCN or ASCO guidelines closely, he or she is not likely to bring up this testing with you. If you’d like to consider chemosensitivity testing, you may need to take the initiative. First, you will need to preplan. Live cells need to be prepared and shipped overnight to a special lab, and so you must discuss this with your doctor before your tumor tissue is removed. For information about this see Standard and Non-Standard Diagnostic Approaches. Knowing how your cancer behaves may influence the type of testing and treatment used, prepare you for possible treatment side effects and guide you in steps to prevent or minimize these effects. It will help you understand and choose the complementary therapies and lifestyle approaches that may enhance your conventional treatment, manage side effects and improve your quality of your life. BCCT advisor Dr. Keith Block relates a case of a patient with recurrent ovarian cancer with chemo-resistance and a high CA-125 level. Block’s team arranged for a tumor biopsy which was assessed by the Nagourney Cancer Institute. Test results showed the tumor was sensitive to a combination of two chemotherapy drugs—even though her tumor had shown resistance to both drugs when used individually. Within two months of starting the drug combination, her CA-125 level dropped significantly and her disease stabilized. Block states he would never have come up with this combination if not for the testing.55 |
Beyond the 7 Healing Practices: Further Integrative Therapies
Complementary Approaches in Ovarian Cancer: Involving Conventional Healthcare ProvidersA 2018 review of complementary treatments for gynecologic cancer found these rates of use and communication between patients and healthcare providers:56
|
Conventional treatments are readily available and are discussed below. Complementary therapies can be useful to enhance conventional treatment effects, improve quality of life and possibly even extend life for those with ovarian cancer. Many complementary therapies―when chosen thoughtfully, reviewed with your oncology treatment team and used alongside conventional therapies—can become part of your integrative cancer care approach.
Therapies are grouped according to their effects:
- Treating the cancer
- Managing side effects and promoting wellness
- Reducing risk
- Optimizing your terrain
We present natural products in six groups:
- Good clinical evidence of efficacy & safety, easy access
- Good clinical evidence of efficacy & safety, limited access
- Limited clinical evidence of efficacy but good safety, used in leading integrative programs
- Limited clinical evidence of efficacy, or significant cautions, but potential significant benefit
- Especially promising preclinical or emerging clinical evidence of efficacy and safety
- Evidence of no efficacy or may be dangerous
Off-label, overlooked and novel cancer approaches (ONCAs) are grouped separately:
- Group A: Good clinical evidence of efficacy
- Group B: Limited clinical evidence of efficacy
- Group C: Promising preclinical evidence only
- Group D: Evidence of no efficacy or may be dangerous
Other integrative therapies and approaches are described but not categorized. See the full summaries as linked for more information on each of these therapies.
Treating the Cancer
Working against cancer growth or spread, improving survival, or working with other treatments or therapies to improve their anticancer action
Conventional Treatments
Integrative Approaches and SurgerySurgery may be part of the recommended treatment for this cancer type. We provide helpful information about how integrative approaches can coordinate with surgery on our Integrative Approaches and Surgery page. |
In general, the earlier the stage of the cancer, the better the response to treatment. Unfortunately, ovarian cancer is typically diagnosed in more advanced stages, which is why treatments are less effective.
The most common primary conventional treatments for ovarian cancer are surgery, chemotherapy and targeted therapy. Radiation therapy is not typically used as a first-line treatment but may be used for small localized recurrent tumors. Hormone therapy may be prescribed for relapsed low-grade tumors.
Some newer therapies and their outcomes:
- Pressurised intraperitoneal aerosol chemotherapy (PIPAC) is a relatively new treatment for patients with peritoneal metastases. A 2019 review found that an objective clinical response of 62–88 percent was reported for patients with ovarian cancer (median survival of 11–14 months) with PIPAC. Repeated PIPAC did not have a negative effect on quality of life.57
- Pulsed low-dose rate radiation therapy (PLDR-RT) delivers conventional radiation doses in pulses of small doses with intermittent pauses. A small study involved PLDR-RT for patients with gynecologic and other cancers of the pelvis. Patients had undergone radiation therapy to the pelvis previously. Twenty-three patients were treated with a curative intent and 15 were treated palliatively. At one-year, 59 percent of patients treated for curative intent had a clinical, biochemical or radiographic response, and six of the 23 patients had no evidence of disease at their last follow-up. Among the patients treated palliatively, 61 percent had a clinical or radiographic response.58
- Percutaneous thermal ablation (TA) uses either heat, cold or a chemical to destroy cancerous tissue in a target organ. A special type of needle is advanced directly into a tumor within the target organ, guided by ultrasound, computerized tomography (CT) scan and/or X-ray.59 A single session was safe and highly effective in controlling local tumors in metastatic ovarian cancer.60
Sometimes adjustments in how conventional treatments are applied can impact outcomes. A 2011 retrospective analysis suggested that epidural anesthesia and analgesia for ovarian serous adenocarcinoma surgery may reduce mortality during the initial years of follow-up compared to general anesthesia (GA) and intravenous opioid analgesia.61
We recommend these resources to introduce the science and conventional therapies:
Natural Products
Traditional Medicine TherapiesThroughout this summary, you will find examples of therapies used by and in many cases created by traditional medical systems. Foods and herbs such as medicinal mushrooms, soy and curcumin are part of traditional systems. Evidence shows that herbs used in traditional Chinese medicine (TCM) may help in maintaining immune function in women with ovarian cancer. Mind-body practices such as mindfulness meditation and yoga also have roots in these systems. Acupuncture, another approach that is part of the Chinese and Korean medicine traditions, has helped those with ovarian cancer manage symptoms such as nausea. |
“While many herbals have been shown to have anticancer properties, the research to date has been largely preclinical (in vitro), without clinical evidence of their effectiveness.”62 Here we make clear the level of evidence behind natural products.
Group 1: Good clinical evidence of efficacy & safety, easy access
| Therapy | Notes |
|---|---|
| Combination therapy of Indole 3-carbinol (I3C) (About Herbs) and EGCG | Improved survival, progression-free survival, performance scores and quality of life when used prior to and during combined treatment, including neoadjuvant (prior to surgery) platinum-taxane chemotherapy, surgery, and adjuvant (supplemental) platinum-taxane chemotherapy63 |
Group 3: Limited clinical evidence of efficacy but good safety, used in leading integrative programs
| Therapy | Notes |
|---|---|
| Melatonin |
|
| Mistletoe (Viscum album) |
|
|
Group 4: Potential significant benefit, but either limited clinical evidence of efficacy or significant cautions
May be used in leading integrative oncology programs. Therapies in this group may need more medical oversight and surveillance.
| Therapy | Notes |
|---|---|
| Combinations of therapies |
|
| Glutathione |
|
| Intravenous vitamin C |
|
Other therapies with preclinical evidence only for treating the cancer
|
Group 5: Especially promising preclinical or emerging clinical evidence of efficacy and safety
| Therapy | Notes |
|---|---|
| Agaricus blazei Murill mushroom | |
| Ashwagandha (Withaferin A) |
|
|
|
| Combinations of therapies |
|
| Flaxseed |
|
| Lycopene supplements |
|
| Milk thistle components |
|
| Nicotinamide (About Herbs) (a form of vitamin B3, also known as niacinamide) | |
| Quercetin | |
| Selenium |
Group 6: Evidence of no efficacy or may be dangerous
| Therapy | Notes |
|---|---|
| Ginseng (About Herbs) |
|
| Vitamin D supplements |
|
Off-label, Overlooked or Novel Cancer Approaches (ONCAs)
These therapies have exciting potential and/or proven benefits. However, some carry higher risks of side effects, interactions with other treatments and other adverse medical events than other therapies we review. Cautions are noted with each therapy, and we strongly encourage you to consult your doctor before using these therapies—even over-the-counter drugs—for cancer treatment. We also note whether a prescription is needed or if a therapy is not widely available.
Group A: Good clinical evidence of efficacy
May be used in integrative protocols and programs
| Therapy | Notes |
|---|---|
| Beta blockers |
|
| Chronomodulated treatment |
|
| Metformin |
|
Group B: Limited clinical evidence of efficacy
May be used in integrative protocols and programs
| Therapy | Notes |
|---|---|
|
Copper chelation using tetrathiomolybdate or other chelators |
|
|
Non-steroidal anti-inflammatory drugs (NSAIDs) including aspirin and COXII inhibitors |
|
|
Group C: Promising preclinical evidence only
| Therapy | Notes |
|---|---|
|
|
|
|
|
Therapies using heat, sound or light
Hyperthermia
- Hyperthermic intraperitoneal chemotherapy (HIPEC)
- Cytoreductive surgery combined with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) is recommended by the Peritoneal Surface Oncology Group International for ovarian cancer.133
- Improved overall survival rates for both primary and recurrent epithelial ovarian cancer (EOC) in several reviews134
- Other reviews concluded that evidence to date is insufficient to support a general recommendation for use in ovarian cancer.135
- Whole-body hyperthermia
- Small clinical trials have found isolated cases of complete remission, extended survival and other benefits for ovarian cancer patients.136
See Hyperthermia.
Managing Side Effects and Promoting Wellness
Managing or relieving side effects or symptoms, reducing treatment toxicity, supporting quality of life or promoting general well-being
Sexual Activity, Depression and Ovarian CancerA number of sexual difficulties can arise if ovarian cancer treatment causes hormonal changes:
Focus on survival can lead to a lack of interest in sex. Symptoms, including depression, anxiety and fatigue can also lead to sexual difficulties. Your oncology care team should ask about changes in sexual function since your diagnosis, but if you haven't been asked about or prepared for managing potential sexual difficulties, ask your doctor about this. For providers uncomfortable with management, a number of programs in sexuality after cancer are available at tertiary care centers.137 A study of sexual activity and functioning of epithelial ovarian cancer survivors (EOCSs) found patterns regarding sexual activity, sexual pleasure and sexual discomfort:138
Because sexual activity and pleasure contribute to survivors’ quality of life, the researchers suggest that healthcare professionals be mindful of sexual health and function, informing and treating patients as indicated. See Sexual Difficulties. |
Conventional Treatments
A study of sexual activity and functioning of epithelial ovarian cancer survivors found that “low estrogen levels were significantly associated with sexual discomfort.”139 Vaginal moisturizers and vaginal rings supplying low-dose estrogen are used to address sexual discomfort and difficulties. Although these are conventional therapies, they may not be included in many conventional treatment programs unless or until a patient expresses a need.
Hormone replacement therapy (HRT) is used for hot flashes and sexual discomfort that arise with ovarian cancer and treatments.
A combination regimen of megestrol acetate (MA) plus L-carnitine, celecoxib (a non-steroidal anti-inflammatory drug) and antioxidants has shown these effects:140
- Improved metabolism and inflammation as well as lean body mass, resting energy expenditure, fatigue and overall quality of life compared to MA alone
- Improved appetite and performance status (a measure of physical function) compared to MA alone
Pulsed low-dose rate radiation therapy (PLDR-RT) delivers conventional radiation doses in pulses of small doses with intermittent pauses. A small study involved PLDR-RT for ovarian and other cancers of the pelvis. Of the 50 percent of patients who reported pain at the local site before treatment, 68 percent reported an improvement in pain after PLDT-RT.141
Natural Products
Group 1: Good clinical evidence of efficacy & safety, easy access
These therapies may be widely used in integrative cancer protocols and traditional medical systems.
| Therapy | Notes |
|---|---|
|
|
|
|
|
Panax ginseng (About Herbs) |
|
| Reduced peripheral neuropathy in several small clinical studies, one of which used alpha-tocopherol (a form of vitamin E)150 |
Group 2: Good clinical evidence of efficacy & safety, limited access
Some may require a prescription, for example.
| Therapy | Notes |
|---|---|
|
Group 3: Limited clinical evidence of efficacy but good safety, used in leading integrative programs
| Therapy | Notes |
|---|---|
|
Individualized homeopathy |
|
|
Mistletoe (Viscum album) |
|
Group 4: Potential significant benefit, but either limited clinical evidence of efficacy or significant cautions
May be used in leading integrative oncology programs. Therapies in this group may need more medical oversight and surveillance.
| Therapy | Notes |
|---|---|
|
|
|
Combinations of therapies |
|
|
Ginkgo biloba (About Herbs) |
|
|
Glutathione (About Herbs) |
|
|
Intravenous vitamin C |
|
|
|
|
Red ginseng (About Herbs) |
|
| Selenium |
|
Group 5: Especially promising preclinical or emerging clinical evidence of efficacy and safety
| Therapy | Notes |
|---|---|
|
|
|
Off-label, Overlooked or Novel Cancer Approaches (ONCAs)
These therapies have exciting potential and/or proven benefits. However, some carry higher risks of side effects, interactions with other treatments and other adverse medical events than other therapies we review. Cautions are noted with each therapy, and we strongly urge you consult your doctor before using these therapies—even over-the-counter drugs—for cancer treatment. We also note whether a prescription is needed or if a therapy is not widely available.
Group C: Promising preclinical evidence only
| Therapy | Notes |
|---|---|
|
|
|
Energy Therapies
Healing Touch
- No evidence of improvements in quality of life with hypnosis, therapeutic massage and healing touch with each cycle of chemotherapy181
Mind-Body, Spiritual and Consciousness-changing Approaches
Training, Relaxation and/or Behavioral therapy
- Improved overall sexual functioning and psychological distress that was maintained at a six-month follow-up182
- Improved symptoms of anxiety and personality development, but not major depression183
- Reduced anxiety, with psycho-oncology therapy slightly more effective than a single relaxation intervention in preventing depression184
Hypnosis
- Reduced pain185
- No evidence of improvements in quality of life with each cycle of chemotherapy when combined with therapeutic massage and healing touch186
Yoga
- Improved depression, negative affect (emotional state), state anxiety (anxiety in response to a specific situation), mental health and overall quality of life, with decreases in fatigue187
See Mind-Body Approaches and Yoga.
Manipulative and Body-Based Methods
Acupuncture
- Improved social function, but not symptoms of pain or insomnia (preliminary evidence)188
- Prevented immediate-onset vomiting following carboplatin-paclitaxel chemotherapy; as effective as the anti-nausea drug ondansetron for immediate-onset vomiting and superior to ondansetron in preventing delayed vomiting at days four and five. The acupuncture-treated group also reported less insomnia and constipation and better general quality-of-life scores.189
- Lower frequency of nausea and incidence of constipation in patients treated by chemotherapy when combined with ginger moxibustion, plus fewer side effects, lower cost, and less risk than the control therapy of intravenous tropisetron hydrochloride and dexamethasone190
See Acupuncture.
Massage Therapy
- Clinical practice guidelines:
- The 2016 American Society of Clinical Oncology clinical practice guideline for managing chronic pain in survivors of adult cancers makes a weak recommendation for using massage.191
- The patient-education resource from the American Society for Clinical Oncology (ASCO) advises an integrative approach including massage to manage peripheral neuropathy.192
- Reduced feelings of hopelessness in ovarian cancer patients undergoing treatment193
- Reduced severity of subjective physical complaints and reduced urinary epinephrine, a marker of stress following Anma therapy (Japanese massage) in gynecologic cancer survivors194
- No evidence of improvements in quality of life with hypnosis, therapeutic massage and healing touch with each cycle of chemotherapy195
- The National Cancer Institute urges massage therapists to take precautions with all cancer patients and avoid massaging specific vulnerable areas of the body. In addition, certain patients with multiple bone metastases may be at risk for fracture during deep massage.196
See Massage Therapy.
Diets and Metabolic Therapies
Fasting
- Fasting from 36 hours before to 24 hours after chemotherapy (60-hour fast) improved quality of life and fatigue during chemotherapy.197
- Preliminary evidence (not yet peer-reviewed) found that a 48-hour, water-only fast at the time of each chemotherapy cycle was well tolerated without increasing weight loss, hospital admissions or chemotherapy dose reduction or delays. Patients did not see an improvement in quality of life, but the fasting patients needed only half as many treatment modifications as the nonfasting group.198
- Fasting reduced chemotherapy side effects of neutropenia (low count of white blood cells called neutrophils) and thrombocytopenia (low count of platelets) in a patient with ovarian cancer.199
- See a recommendation from Dr. Lise Alschuler in Commentary below.
Reducing Risk
Reducing the risk of developing cancer or the risk of recurrence
Managing ThrombosisOvarian cancer brings a high risk of formation of blood clots (thrombosis).200 For prevention, BCCT advisor Dr. Keith Block provides information on modifying the terrain factor he calls hypercoagulation.201 He discusses testing, lifestyle approaches and supplements to reduce risks. For more information see chapter 17, “Blood Circulation and Cancer: The Thick and the Thin.” |
Risk Factors
Risk factors for ovarian cancer that are generally not under a woman’s control:202
- Family history of ovarian cancer or BRCA1 and BRCA2 mutation (these mutations are responsible for most family history incidence)
- Age and menopause status
- Greater genetically predicted adult height
- Greater number of menstrual cycles, influenced by early menarche, late menopause, fewer pregnancies or periods of lactation or contraceptive use
- Infertility
- Personal history of breast cancer
Lifestyle Associations
Increased Risk
Risk factors that may be influenced by a woman’s lifestyle choices and behaviors:203
- Smoking tobacco with (borderline) mucinous cancers
- Use of hormone replacement therapy (estrogen plus progesterone) for serous and endometrioid ovarian cancers
- Breastfeeding is modestly associated with a decreased risk of premenopausal ovarian cancer for the mother, likely related to fewer menstrual cycles.
- Lack of physical activity (limited evidence)
- Being overweight or obese (inconsistent evidence)
An extensive meta-analysis did not find an overall association between ever-exposure to night-shift work and the risk of ovarian cancer.204 However, other evidence shows that rotating between night shifts and day or evening shifts, especially for many years, is linked to higher risk of ovarian cancer, and especially fatal cancer.205
Some initial evidence shows that the microbiome in the cervix and vagina may relate to or indicate ovarian cancer risk. Lower levels of the protective bacteria Lactobacillus in the microbiota in the cervix was associated with higher incidence of ovarian cancer or BRCA1 mutation status, especially in younger women. The research is too preliminary to draw a causal relationship, and no evidence yet shows that restoring the Lactobacillus microbiota in the cervix/vagina might lower the risk.206
Decreased Risk
Oral contraceptive use has shown a protective effect against ovarian cancer and may last several decades after use is discontinued. Use was also associated with a slightly increased risk of breast cancer, but this increase disappeared a few years after use was discontinued.207
Natural Products
Group 1: Good clinical evidence of efficacy & safety, easy access
These therapies may be widely used in integrative cancer protocols and traditional medical systems.
| Therapy | Notes |
|---|---|
|
Isoflavones, including genistein from soy Benefits of soy foods are discussed above in Eating Well |
|
|
Group 3: Limited clinical evidence of efficacy but good safety, used in leading integrative programs
| Therapy | Notes |
|---|---|
|
Combined therapies |
|
|
Intravenous, high-dose vitamin C |
|
Group 4: Potential significant benefit, but either limited clinical evidence of efficacy or significant cautions
May be used in leading integrative oncology programs. Therapies in this group may need more medical oversight and surveillance.
| Therapy | Notes |
|---|---|
|
Ginkgo biloba (About Herbs) |
|
Group 5: Especially promising preclinical or emerging clinical evidence of efficacy and safety
Other therapies with preclinical evidence only for reducing risk
|
| Therapy | Notes |
|---|---|
|
|
|
Lycopene supplements |
|
Group 6: Evidence of no efficacy or may be dangerous
| Therapy | Notes |
|---|---|
|
|
|
Oral vitamin C |
|
|
Vitamin D supplements |
|
Off-label, Overlooked or Novel Cancer Approaches (ONCAs)
These therapies have exciting potential and/or proven benefits. However, some carry higher risks of side effects, interactions with other treatments and other adverse medical events than other therapies we review. Cautions are noted with each therapy, and we strongly urge you consult your doctor before using these therapies—even over-the-counter drugs—for cancer treatment. We also note whether a prescription is needed or if a therapy is not widely available.
Group B: Limited clinical evidence of efficacy
| Therapy | Notes |
|---|---|
|
Non-steroidal anti-inflammatory drugs (NSAIDs) including aspirin and COXII inhibitors |
|
|
Optimizing Your Terrain
Creating an environment within your body that does not support cancer development, growth or spread
Natural Products
Group 1: Good clinical evidence of efficacy & safety, easy access
| Therapy | Notes |
|---|---|
|
|
|
Group 3: Limited clinical evidence of efficacy but good safety, used in leading integrative programs
| Therapy | Notes |
|---|---|
| Bromelain (About Herbs) |
|
| Isoflavones, including genistein from soy |
|
Group 4: Potential significant benefit, but either limited clinical evidence of efficacy or significant cautions
May be used in leading integrative oncology programs. Therapies in this group may need more medical oversight and surveillance.
| Therapy | Notes |
|---|---|
| Agaricus blazei Murill mushroom |
|
Group 5: Especially promising preclinical or emerging clinical evidence of efficacy and safety
| Therapy | Notes |
|---|---|
|
Turkey tail mushroom polysaccarides (PSK ) |
|
Energy Therapies
Healing Touch
- Trends of higher levels of immune modulators (CD4, CD8 and natural killer (NK) cells) with healing touch in combination with therapeutic massage and hypnosis with each cycle of chemotherapy243
See Healing Touch.
Manipulative and Body-Based Methods
Acupuncture
- Higher white blood cell counts during one cycle of chemotherapy (modest evidence)244
Massage
- Trends of higher levels of immune modulators (CD4, CD8 and natural killer (NK) cells) with therapeutic massage in combination with hypnosis and healing touch with each cycle of chemotherapy245
Mind-Body, Spiritual and Consciousness-changing Approaches
Hypnosis
- Trends of higher levels of immune modulators (CD4, CD8 and natural killer (NK) cells) with hypnosis in combination with therapeutic massage and healing touch with each cycle of chemotherapy246
See Mind-Body Approaches.
Commentary
Fasting
For people having significant side effects, especially gastrointestinal, from chemo, naturopathic oncologist and BCCT advisor Lise Alschuler recommends fasting for 48 hours—from after dinner on the day before chemo, through the day of chemo and the day following chemotherapy. The chemo fast can be a water fast (which includes coconut water and vegetable broths), or you can eat up to 600 calories per day of vegetable soup and/or low-carb vegetables. She stresses the importance of your being motivated to fast, and also that fasting during chemotherapy should be cleared with your treating oncologist. You should modify or stop the fast if you become dizzy or weak (try adding boiled eggs or nuts), or if you feel worse than if you had eaten.
Eggs
Dr. Alschuler and her colleague Karolyn Gazella advise people with risk for ovarian to consider limiting egg intake to fewer than five eggs a week, while choosing eggs from free-roaming, organically fed chickens. They also advise boiling or poaching eggs, as these methods do not oxidize the yolk fat.247
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889.
- Nelson R. Can integrative oncology extend life in advanced disease? Medscape Medical News. October 25, 2013. Viewed February 1, 2019.
- Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Ovarian Cancer. Viewed February 8, 2019.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016. p. 316.
- Ben-Arye E, Schiff E, Steiner M, Keshet Y, Lavie O. Attitudes of patients with gynecological and breast cancer toward integration of complementary medicine in cancer care. International Journal of Gynecological Cancer. 2012;22(1):146‐153.
- Ben-Arye B. Integrative Gynecologic Oncology--would value your input [personal email communication with Laura Pole]. May 27, 2020.
- Shalom-Sharabi I, Lavie O, Samuels N, Keinan-Boker L, Lev E, Ben-Arye E. Can complementary medicine increase adherence to chemotherapy dosing protocol? A controlled study in an integrative oncology setting. Journal of Cancer Research and Clinical Oncology. 2017;143(12):2535‐2543.
- Shalom-Sharabi I, Samuels N et al. Impact of a complementary/integrative medicine program on the need for supportive cancer care-related medications. Supportive Care in Cancer. 2017;25(10):3181‐3190.
- Ben-Arye E, Samuels N et al. Quality-of-life outcomes in patients with gynecologic cancer referred to integrative oncology treatment during chemotherapy. Supportive Care in Cancer. 2015;23(12):3411‐3419.
- Shalom-Sharabi I, Samuels N et al. Effect of a patient-tailored integrative medicine program on gastro-intestinal concerns and quality of life in patients with breast and gynecologic cancer. Journal of Cancer Research and Clinical Oncology. 2017;143(7):1243‐1254.
- Ben-Arye E, Aharonson ML, Schiff E, Samuels N. Alleviating gastro-intestinal symptoms and concerns by integrating patient-tailored complementary medicine in supportive cancer care. Clinical Nutrition. 2015;34(6):1215‐1223.
- Shalom-Sharabi I, Samuels N et al. Effect of a patient-tailored integrative medicine program on gastro-intestinal concerns and quality of life in patients with breast and gynecologic cancer. Journal of Cancer Research and Clinical Oncology. 2017;143(7):1243‐1254; Ben-Arye E, Samuels N et al. Quality-of-life outcomes in patients with gynecologic cancer referred to integrative oncology treatment during chemotherapy. Supportive Care in Cancer. 2015;23(12):3411‐3419.
- Keshet Y, Schiff E, Samuels N, Ben-Arye E. Giving voice to cancer patients: assessing non-specific effects of an integrative oncology therapeutic program via short patient narratives. Psychooncology. 2015;24(2):169‐174.
- Ben-Arye E, Samuels N, Schiff E, Lavie O. Designing an integrative gynecologic oncology model of supportive care: call for a cross-cultural international collaboration. Supportive Care in Cancer. 2016;24(4):1457‐1458.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Block KI.Life over Cancer: The Block Center Program for Integrative Cancer Treatment. New York: Bantam Dell. 2009.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Chan KK, Yao TJ et al. The use of Chinese herbal medicine to improve quality of life in women undergoing chemotherapy for ovarian cancer: a double-blind placebo-controlled randomized trial with immunological monitoring. Annals of Oncology. 2011 Oct;22(10):2241-9.
- Bae K, Kim E, Choi JJ, Kim MK, Yoo HS. The effectiveness of anticancer traditional Korean medicine treatment on the survival in patients with lung, breast, gastric, colorectal, hepatic, uterine, or ovarian cancer: a prospective cohort study protocol. Medicine (Baltimore). 2018 Oct;97(41):e12444.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889; Playdon MC, Nagle CM et al. Pre-diagnosis diet and survival after a diagnosis of ovarian cancer. British Journal of Cancer. 2017 Jun 6;116(12):1627-1637; Webb PM, de Fazio A et al. Circulating 25-hydroxyvitamin D and survival in women with ovarian cancer. American Journal of Clinical Nutrition. 2015 Jul;102(1):109-14; Ong JS1,2, Cuellar-Partida G et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. International Journal of Epidemiology. 2016 Oct;45(5):1619-1630.
- Playdon MC, Nagle CM et al. Pre-diagnosis diet and survival after a diagnosis of ovarian cancer. British Journal of Cancer. 2017 Jun 6;116(12):1627-1637.
- Wax E, Zieve D. Facts about polyunsaturated fats. Medline Plus. April 30, 2019. Viewed May 7, 2019.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889; Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA. Dietary intake and ovarian cancer risk: a systematic review. Cancer Epidemiology, Biomarkers & Prevention. 2014 Feb;23(2):255-73; Xu H1, Ding Y, Xin X, Wang W, Zhang D. Dietary fiber intake is associated with a reduced risk of ovarian cancer: a dose-response meta-analysis. Nutrition Research. 2018 Sep;57:1-11; Schwab U, Lauritzen L et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food & Nutrition Research. 2014 Jul 10;58; Qiu W, Lu H, Qi Y, Wang X. Dietary fat intake and ovarian cancer risk: a meta-analysis of epidemiological studies. Oncotarget. 2016 Jun 14;7(24):37390-37406; Ganmaa D, Sato A. The possible role of female sex hormones in milk from pregnant cows in the development of breast, ovarian and corpus uteri cancers. Medical Hypotheses. 2005;65(6):1028-37; Larsson SC, Wolk A. Tea consumption and ovarian cancer risk in a population-based cohort. Archives of Internal Medicine. 2005 Dec 12-26;165(22):2683-6; Larsson SC, Giovannucci E, Wolk A. Dietary folate intake and incidence of ovarian cancer: the Swedish Mammography Cohort. Journal of the National Cancer Institute. 2004 Mar 3;96(5):396-402; Silvera SA, Jain M, Howe GR, Miller AB, Rohan TE. Carotenoid, vitamin A, vitamin C, and vitamin E intake and risk of ovarian cancer: a prospective cohort study. Cancer Epidemiology, Biomarkers & Prevention. 2006 Feb;15(2):395-7; Lee AH, Su D et al. Soy and isoflavone intake associated with reduced risk of ovarian cancer in southern Chinese women. Nutrition Research. 2014 Apr;34(4):302-7; Qu XL, Fang Y, Zhang M, Zhang YZ. Phytoestrogen intake and risk of ovarian cancer: a meta- analysis of 10 observational studies. Asian Pacific Journal of Cancer Prevention. 2014;15(21):9085-91; Myung SK, Ju W, Choi HJ, Kim SC; Korean Meta-Analysis (KORMA) Study Group. Soy intake and risk of endocrine-related gynaecological cancer: a meta-analysis. BJOG. 2009 Dec;116(13):1697-705; Tung KH, Wilkens LR et al. Association of dietary vitamin A, carotenoids, and other antioxidants with the risk of ovarian cancer. Cancer Epidemiology, Biomarkers & Prevention. 2005 Mar;14(3):669-76; Jeong NH, Song ES et al. Plasma carotenoids, retinol and tocopherol levels and the risk of ovarian cancer. Acta Obstet Gynecol Scand. 2009;88(4):457-62; Li X, Xu J. Meta-analysis of the association between dietary lycopene intake and ovarian cancer risk in postmenopausal women. Scientific Reports. 2014 May 9;4:4885; Tang L, Lee AH, Su D, Binns CW. Fruit and vegetable consumption associated with reduced risk of epithelial ovarian cancer in southern Chinese women. Gynecologic Oncology. 2014 Jan;132(1):241-7; Gifkins D, Olson SH et al. Total and individual antioxidant intake and risk of epithelial ovarian cancer. BMC Cancer. 2012 Jun 1;12:211; Merritt MA, Cramer DW et al. Dietary fat intake and risk of epithelial ovarian cancer by tumour histology. British Journal of Cancer. 2014 Mar 4;110(5):1392-401; Hoang T, Myung SK, Pham TT. Dietary intake of omega-3 fatty acids and endocrine-related gynecological cancer: a meta-analysis of observational studies. Cancer Research and Treatment. 2018 Oct 17; Leung AC1, Cook LS et al. Tea, coffee, and caffeinated beverage consumption and risk of epithelial ovarian cancers. Cancer Epidemiology. 2016 Dec;45:119-125; Hashibe M, Galeone C et al. Coffee, tea, caffeine intake, and the risk of cancer in the PLCO cohort. British Journal of Cancer. 2015 Sep 1;113(5):809-16.
- Trudel D, Labbé DP et al. A two-stage, single-arm, phase II study of EGCG-enriched green tea drink as a maintenance therapy in women with advanced stage ovarian cancer. Gynecologic Oncology. 2013 Nov;131(2):357-61.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889.
- Tabung FK, Huang T et al. The inflammatory potential of diet and ovarian cancer risk: results from two prospective cohort studies. British Journal of Cancer. 2017 Sep 5;117(6):907-911.
- Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA. Dietary intake and ovarian cancer risk: a systematic review. Cancer Epidemiology, Biomarkers & Prevention. 2014 Feb;23(2):255-73; Keum N, Lee DH et al. Egg intake and cancers of the breast, ovary and prostate: a dose-response meta-analysis of prospective observational studies. British Journal of Nutrition. 2015 Oct 14;114(7):1099-107; Thorning TK, Raben A et al. Milk and dairy products: good or bad for human health? An assessment of the totality of scientific evidence. Food & Nutrition Research. 2016 Nov 22;60:32527; Cancer Epidemiol Biomarkers Prev. 2006 Feb;15(2):395-7; Silvera SA, Jain M, Howe GR, Miller AB, Rohan TE. Carotenoid, vitamin A, vitamin C, and vitamin E intake and risk of ovarian cancer: a prospective cohort study. Cancer Epidemiology, Biomarkers & Prevention. 2006 Feb;15(2):395-7; Jolfaie NR, Rouhani MH, Onvani S, Azadbakht L. The association between vitamin D and health outcomes in women: a review on the related evidence. Journal of Research in Medical Sciences. 2016 Sep 1;21:76. eCollection 2016; Tschernichovsky R, Goodman A et al. Risk-reducing strategies for ovarian cancer in BRCA mutation carriers: a balancing act. Oncologist. 2017 Apr;22(4):450-459; Hashibe M, Galeone C et al. Coffee, tea, caffeine intake, and the risk of cancer in the PLCO cohort. British Journal of Cancer. 2015 Sep 1;113(5):809-16.
- Qu XL, Fang Y, Zhang M, Zhang YZ. Phytoestrogen intake and risk of ovarian cancer: a meta- analysis of 10 observational studies. Asian Pacific Journal of Cancer Prevention. 2014;15(21):9085-91.
- Mulholland HG, Murray LJ, Cardwell CR, Cantwell MM. Dietary glycaemic index, glycaemic load and endometrial and ovarian cancer risk: a systematic review and meta-analysis. British Journal of Cancer. 2008 Aug 5;99(3):434-41.
- Zhang Y, Wu J et al. Association of serum lipids and severity of epithelial ovarian cancer: an observational cohort study of 349 Chinese patients. Journal of Biomedical Research. 2018 Sep 29;32(5):336-342.
- Schofield C, Newton RU, Galvão DA, Cohen PA, Peddle-McIntyre CJ. A physiological profile of ovarian cancer survivors to inform tailored exercise interventions and the development of exercise oncology guidelines. International Journal of Gynecologic Cancer. 2017 Sep;27(7):1560-1567.
- Poole EM, Konstantinopoulos PA, Terry KL. Prognostic implications of reproductive and lifestyle factors in ovarian cancer. Gynecologic Oncology. 2016 Sep;142(3):574-87.
- von Gruenigen VE, Frasure HE et al. Feasibility of a lifestyle intervention for ovarian cancer patients receiving adjuvant chemotherapy. Gynecologic Oncology. 2011 Aug;122(2):328-33.
- Zhang Q, Li F, Zhang H, Yu X, Cong Y. Effects of nurse-led home-based exercise & cognitive behavioral therapy on reducing cancer-related fatigue in patients with ovarian cancer during and after chemotherapy: A randomized controlled trial. International Journal of Nursing Studies. 2018 Feb;78:52-60.
- Crawford JJ, Vallance JK, Holt NL, Courneya KS. Associations between exercise and posttraumatic growth in gynecologic cancer survivors.Supportive Care in Cancer. 2015 Mar;23(3):705-14.
- Smits A, Lopes A et al. The effect of lifestyle interventions on the quality of life of gynaecological cancer survivors: a systematic review and meta-analysis. Gynecologic Oncology. 2015 Dec;139(3):546-52.
- Yeganeh L, Harrison C, Vincent AJ, Teede H, Boyle JA. Effects of lifestyle modification on cancer recurrence, overall survival and quality of life in gynaecological cancer survivors: a systematic review and meta-analysis. Maturitas. 2018 May;111:82-89.
- Beavis AL, Smith AJ, Fader AN. Lifestyle changes and the risk of developing endometrial and ovarian cancers: opportunities for prevention and management. International Journal of Women’s Health. 2016 May 23;8:151-67.
- Fashler SR, Weinrib AZ, Azam MA, Katz J. The use of Acceptance and Commitment Therapy in oncology settings: a narrative review. Psychological Reports. 2018 Apr;121(2):229-252.
- Roberts AL, Huang T et al. Posttraumatic stress disorder (PTSD) is associated with increased risk of ovarian cancer: a prospective and retrospective longitudinal cohort study. Cancer Research. 2019 Sep 5. pii: canres.1222.2019.
- Thaker PH, Lutgendorf SK, Sood AK. The neuroendocrine impact of chronic stress on cancer. Cell Cycle. 2007 Feb 15;6(4):430-3.
- Crane TE, Skiba MB, Donzella S, Thomson CA, Parthasarathy S. 0414 chronotype and sleep among ovarian cancer survivors participating in a lifestyle intervention. Sleep. 2020 April ;43(Supplement_1):A158–A159.
- Hurley S, Goldberg D, Bernstein L, Reynolds P. Sleep duration and cancer risk in women. Cancer Causes & Control. 2015 Jul;26(7):1037-45.
- Penninkilampi R, Eslick GD. Perineal talc use and ovarian cancer: a systematic review and meta-analysis. Epidemiology. 2018 Jan;29(1):41-49.
- Park SH, Kim KY et al. Cell growth of ovarian cancer cells is stimulated by xenoestrogens through an estrogen-dependent pathway, but their stimulation of cell growth appears not to be involved in the activation of the mitogen-activated protein kinases ERK-1 and p38. Journal of Reproduction and Development. 2009 Feb;55(1):23-9.
- Janssen S, Solomon G, Schettler T. Toxicant and Disease Database. Ovarian cancer. Collaborative on Health and the Environment. 2011. Viewed February 3, 2019.
- Janssen S, Solomon G, Schettler T. Toxicant and Disease Database. Ovarian cancer. Collaborative on Health and the Environment. 2011. Viewed February 3, 2019.
- Hill EM, Watkins K et al. Women with ovarian cancer: examining the role of social support and rumination in posttraumatic growth, psychological distress, and psychological well-being. Journal of Clinical Psychology in Medical Settings. 2017 Mar;24(1):47-58.
- Wen Q, Shao Z et al. Mental distress, quality of life and social support in recurrent ovarian cancer patients during active chemotherapy. European Journal of Obstetrics, Gynecology and Reproductive Biology. 2017 Sep;216:85-91.
- Lutgendorf SK, Sood AK et al. Social support, psychological distress, and natural killer cell activity in ovarian cancer. Journal of Clinical Oncology. 2005 Oct 1;23(28):7105-13.
- Idahl A, Hermansson A, Lalos A. Social support and ovarian cancer incidence—a Swedish prospective population-based study. Gynecologic Oncology. 2018 May;149(2):324-328.
- de Moor JS, de Moor CA et al. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosomatic Medicine. 2006 Jul-Aug;68(4):555-62.
- de Moor JS, de Moor CA et al. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosomatic Medicine. 2006 Jul-Aug;68(4):555-62.
- National Comprehensive Cancer Network: Ovarian Cancer: Professional Guidelines (login required). Viewed February 27, 2019.
- Block KI. Life over Cancer: The Block Center Program for Integrative Cancer Treatment. New York: Bantam Dell. 2009. p. 482.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889.
- Alyami M, Hübner M et al. Pressurised intraperitoneal aerosol chemotherapy: rationale, evidence, and potential indications. Lancet Oncology. 2019 Jul;20(7):e368-e377.
- Pulsed low-dose pelvic reirradiation safe, provided tangible benefit for patients with few other options. Fox Chase Cancer Center, September 22, 2020. Viewed September 30, 2020; Paly JJ, Deng M et al. Pelvic reirradiation utilizing pulsed low-dose rate radiation therapy. American Journal of Clinical Oncology. 2020 Oct;43(10):748-751.
- Percutaneous Thermal Ablation. NorthShore University HealthSystem. Viewed April 22, 2021.
- Yuan F, Wei SH et al. Image-guided percutaneous thermal ablation of oligometastatic ovarian and non-ovarian gynecologic tumors. Journal of Vascular and Interventional Radiology. 2021 Feb 16:S1051-0443(21)00315-8.
- Lin L, Liu C et al. Anaesthetic technique may affect prognosis for ovarian serous adenocarcinoma: a retrospective analysis. British Journal of Anaesthesia. 2011 Jun;106(6):814-22.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10): 882.
- Kiselev VI, Ashrafyan LA et al. A new promising way of maintenance therapy in advanced ovarian cancer: a comparative clinical study. BMC Cancer. 2018 Sep 20;18(1):904.
- Chuffa LGA, Reiter RJ, Lupi LA. Melatonin as a promising agent to treat ovarian cancer: molecular mechanisms. Carcinogenesis. 2017 Oct 1;38(10):945-952; de Almeida Chuffa LG, Seiva FRF et al. Mitochondrial functions and melatonin: a tour of the reproductive cancers. Cellular and Molecular Life Sciences. 2018 Nov 14.
- Kim JH, Jeong SJ et al. Melatonin synergistically enhances cisplatin-induced apoptosis via the dephosphorylation of ERK/p90 ribosomal S6 kinase/heat shock protein 27 in SK-OV-3 cells. Journal of Pineal Research. 2012 Mar;52(2):244-52; Lissoni P, Paolorossi F et al. A phase II study of tamoxifen plus melatonin in metastatic solid tumour patients. British Journal of Cancer. 1996 Nov;74(9):1466-8.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Freuding M, Keinki C, Micke O, Buentzel J, Huebner J. Mistletoe in oncological treatment: a systematic review: part 1:survival and safety. Journal of Cancer Research and Clinical Oncology. 2019 Jan 23.
- Grossarth-Maticek R, Ziegler R. Prospective controlled cohort studies on long-term therapy of ovarian cancer patients with mistletoe (Viscum album L.) extracts Iscador. Arzneimittelforschung. 2007;57(10):665-78.
- Kienle GS, Glockmann A, Schink M, Kiene H. Viscum album L. extracts in breast and gynaecological cancers: a systematic review of clinical and preclinical research. Journal of Experimental and Clinical Cancer Research. 2009 Jun 11;28:79.
- Ben-Arye E, Lavie O. Safety of herbal medicine use during chemotherapy in patients with ovarian cancer: a "bedside-to-bench" approach. Med Oncol. 2017 Apr;34(4):54.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Fujimoto K, Tomonaga M, Goto S. A case of recurrent ovarian cancer successfully treated with adoptive immunotherapy and lentinan. Anticancer Research. 2006 Nov-Dec;26(6A):4015-8.
- Shimizu Y, Hasumi K et al. [Successful treatment of a patient with recurrent ovarian cancer by lentinan combined with intraarterial 5FU]. [Article in Japanese] Nihon Gan Chiryo Gakkai Shi. 1989 Mar 20;24(3):647-51.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Schwartz L, Buhler L, Icard P, Lincet H, Steyaert JM. Metabolic treatment of cancer: intermediate results of a prospective case series. Anticancer Research. 2014 Feb;34(2):973-80.
- Drisko JA, Chapman J, Hunter VJ. The use of antioxidants with first-line chemotherapy in two cases of ovarian cancer. Journal of the American College of Nutrition. 2003 Apr;22(2):118-23.
- Bohm S, Oriana S et al. Dose intensification of platinum compounds with glutathione protection as induction chemotherapy for advanced ovarian carcinoma, Oncology 1999; 57(2):115-120.
- Nunes SC, Serpa J. Glutathione in ovarian cancer: a double-edged sword. International Journal of Molecular Sciences. 2018 Jun 26;19(7). pii: E1882.
- Nauman G, Gray JC, Parkinson R, Levine M, Paller CJ. Systematic review of intravenous ascorbate in cancer clinical trials. Antioxidants (Basel). 2018 Jul 12;7(7):89.
- Ma Y, Chapman J et al. High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Science Translational Medicine. 2014 Feb 5;6(222):222ra18.
- Chen Q, Espey MG et al. Pharmacologic doses of ascorbate act as a prooxidant and decrease growth of aggressive tumor xenografts in mice. Proceedings of the National Academy of Sciences U S A. 2008 Aug 12;105(32):11105-9.
- Kobayashi H, Yoshida R et al. Suppressing effects of daily oral supplementation of beta-glucan extracted from Agaricus blazei Murill on spontaneous and peritoneal disseminated metastasis in mouse model. Journal of Cancer Research and Clinical Oncology. 2005 Aug;131(8):527-38.
- Mukai H, Watanabe T, Ando M, Katsumata N. An alternative medicine, Agaricus blazei, may have induced severe hepatic dysfunction in cancer patients. Japanese Journal of Clinical Oncology. 2006 Dec;36(12):808-10.
- Kakar SS, Ratajczak MZ et al. Withaferin a alone and in combination with cisplatin suppresses growth and metastasis of ovarian cancer by targeting putative cancer stem cells. PLoS One. 2014 Sep 29;9(9):e107596.
- Chu Z, Wang Z, Liu T, Xiong S, Liu B. Evaluation of the effects of astragalus membranaceus on the pharmacokinetics of pemetrexed disodium and gemcitabine in rats by a simple high-performance liquid chromatography/UV method. Journal of Analytical Methods in Chemistry. 2019 Apr 28;2019:3162426.
- Zhao J, Pan Y et al. Dihydroartemisinin and curcumin synergistically induce apoptosis in SKOV3 cells via upregulation of MiR-124 targeting midkine. Cell Physiology and Biochemistry. 2017;43(2):589-601.
- Dikshit A, Hales K, Hales DB. Whole flaxseed diet alters estrogen metabolism to promote 2-methoxtestradiol-induced apoptosis in hen ovarian cancer. Journal of Nutritional Biochemistry. 2017 Apr;42:117-125.
- Holzapfel NP, Shokoohmand A et al. Lycopene reduces ovarian tumor growth and intraperitoneal metastatic load. American Journal of Cancer Research. 2017 Jun 1;7(6):1322-1336. eCollection 2017.
- Cho HJ, Suh DS et al. Silibinin inhibits tumor growth through downregulation of extracellular signal-regulated kinase and Akt in vitro and in vivo in human ovarian cancer cells. Journal of Agricultural and Food Chemistry. 2013 May 1;61(17):4089-96.
- Pashaei-Asl F, Pashaei-Asl R et al. Enhancement of anticancer activity by silibinin and paclitaxel combination on the ovarian cancer. Artificial Cells, Nanomedicine and Biotechnology. 2018 Nov;46(7):1483-1487.
- Momeny M, Ghasemi R et al. Effects of silibinin on growth and invasive properties of human ovarian carcinoma cells through suppression of heregulin/HER3 pathway. Tumour Biol. 2016 Mar;37(3):3913-23; Fan L, Ma Y, Liu Y, Zheng D, Huang G. Silymarin induces cell cycle arrest and apoptosis in ovarian cancer cells. European Journal of Pharmacology. 2014 Nov 15;743:79-88.
- Scambia G, De Vincenzo R et al. Antiproliferative effect of silybin on gynaecological malignancies: synergism with cisplatin and doxorubicin. European Journal of Cancer. 1996 May;32A(5):877-82.
- Amawi H, Hussein NA et al. HM015k, a novel silybin derivative, multi-targets metastatic ovarian cancer cells and is safe in zebrafish toxicity studies. Frontiers in Pharmacology. 2017 Aug 2;8:498.
- Horsman MR, Brown JM et al. Mechanism of action of the selective tumor radiosensitizer nicotinamide. International Journal of Radiation Oncology, Biology, Physics. 1988 Sep;15(3):685-90.
- Horsman MR, Siemann DW, Chaplin DJ, Overgaard J. Nicotinamide as a radiosensitizer in tumours and normal tissues: the importance of drug dose and timing. Radiotherapy and Oncology. 1997 Nov;45(2):167-74.
- Liu Y, Gong W et al. Quercetin induces protective autophagy and apoptosis through ER stress via the p-STAT3/Bcl-2 axis in ovarian cancer. Apoptosis. 2017 Apr;22(4):544-557; Hashemzaei M, Delarami Far A et al. Anticancer and apoptosis‑inducing effects of quercetin in vitro and in vivo. Oncology Reports. 2017 Aug;38(2):819-828.
- Parvaresh A, Razavi R et al. Quercetin and ovarian cancer: an evaluation based on a systematic review. Journal of Research in Medical Sciences. 2016 May 9;21:34. eCollection 2016.
- Shen F, Herenyiova M, Weber G. Synergistic down-regulation of signal transduction and cytotoxicity by tiazofurin and quercetin in human ovarian carcinoma cells. Life Sciences. 1999;64(21):1869-76.
- Chen SS, Michael A, Butler-Manuel SA. Advances in the treatment of ovarian cancer: a potential role of antiinflammatory phytochemicals. Discovery Medicine. 2012 Jan;13(68):7-17.
- Frenkel GD, Caffrey PB. A prevention strategy for circumventing drug resistance in cancer chemotherapy. Current Pharmaceutical Design. 2001 Nov;7(16):1595-614.
- Evans SO, Khairuddin PF, Jameson MB. Optimising selenium for modulation of cancer treatments..Anticancer Research. 2017 Dec;37(12):6497-6509.
- Kim HS, Kim MK et al. Effect of red ginseng on genotoxicity and health-related quality of life after adjuvant chemotherapy in patients with epithelial ovarian cancer: a randomized, double blind, placebo-controlled trial. Nutrients. 2017 Jul 19;9(7). pii: E772.
- Jeffreys M, Redaniel MT, Martin RM. The effect of pre-diagnostic vitamin D supplementation on cancer survival in women: a cohort study within the UK Clinical Practice Research Datalink. BMC Cancer. 2015 Oct 12;15:670.
- Hefner J, Csef H et al. The clinical relevance of beta blockers in ovarian carcinoma: a systematic review. Geburtshilfe und Frauenheilkunde. 2016 Oct;76(10):1050-1056.
- Kobayashi M, Wood PA, Hrushesky WJ. Circadian chemotherapy for gynecological and genitourinary cancers. Chronobiology International. 2002 Jan;19(1):237-51.
- Kumar S, Meuter A et al. Metformin intake is associated with better survival in ovarian cancer: a case-control study. Cancer. 2013;119:555–562.
- Currie CJ, Poole CD et al. Mortality after incident cancer in people with and without type 2 diabetes: impact of metformin on survival. Diabetes Care. 2012;35(2):299-304.
- Lengyel E, Litchfield LM et al. Metformin inhibits ovarian cancer growth and increases sensitivity to paclitaxel in mouse models. American Journal of Obstetrics and Gynecology. 2015 Apr;212(4):479.e1-479.e10.
- Hijaz M, Chhina J et al. Preclinical evaluation of olaparib and metformin combination in BRCA1 wildtype ovarian cancer. Gynecologic Oncology. 2016 Aug;142(2):323-31.
- Mert I, Chhina J et al. Synergistic effect of MEK inhibitor and metformin combination in low grade serous ovarian cancer. Gynecologic Oncology. 2017 Aug;146(2):319-326.
- Chen HH, Chen WC et al. Targeting drug transport mechanisms for improving platinum-based cancer chemotherapy. Expert Opinion on Therapeutic Targets. 2015;19(10):1307-17; Chen HH, Kuo MT. Overcoming platinum drug resistance with copper-lowering agents. Anticancer Research. 2013 Oct;33(10):4157-61.
- Ishida S, McCormick F, Smith-McCune K, Hanahan D. Enhancing tumor-specific uptake of the anticancer drug cisplatin with a copper chelator. Cancer Cell. 2010 Jun 15;17(6):574-83.
- Kim KK, Lange TS, Singh RK, Brard L, Moore RG. Tetrathiomolybdate sensitizes ovarian cancer cells to anticancer drugs doxorubicin, fenretinide, 5-fluorouracil and mitomycin C. BMC Cancer. 2012 Apr 13;12:147.
- Verdoodt F, Dehlendorff C, Friis S, Kjaer SK. Non-aspirin NSAID use and ovarian cancer mortality. Gynecologic Oncology. 2018 Aug;150(2):331-337.
- Merritt MA, Rice MS et al. Pre-diagnosis and post-diagnosis use of common analgesics and ovarian cancer prognosis (NHS/NHSII): a cohort study. Lancet Oncology. 2018 Aug;19(8):1107-1116.
- Pantziarka P, Sukhatme V, Bouche G, Meheus L, Sukhatme VP. Repurposing Drugs in Oncology (ReDO)-diclofenac as an anti-cancer agent. Ecancermedicalscience. 2016;10:610.
- Verdoodt F, Kjaer SK, Friis S. Influence of aspirin and non-aspirin NSAID use on ovarian and endometrial cancer: summary of epidemiologic evidence of cancer risk and prognosis. Maturitas. 2017 Jun;100:1-7.
- Huang Y, Lichtenberger LM et al. Antitumor and antiangiogenic effects of aspirin-PC in ovarian cancer. Molecular Cancer Therapeutics. 2016 Dec;15(12):2894-2904.
- Pantziarka P, Sukhatme V, Bouche G, Meheus L, Sukhatme VP. Repurposing Drugs in Oncology (ReDO)-diclofenac as an anti-cancer agent. Ecancermedicalscience. 2016;10:610.
- Khan MS, Fatima K, Rameez. Impact of statins on risk and survival of ovarian cancer. Journal of Gynecologic Oncology. 2015 Jul;26(3):240-1; Urpilainen E, Marttila M et al. Prognosis of ovarian cancer in women with type 2 diabetes using metformin and other forms of antidiabetic medication or statins: a retrospective cohort study. BMC Cancer. 2018 Jul 28;18(1):767; Verdoodt F, Kjaer Hansen M et al. Statin use and mortality among ovarian cancer patients: a population-based cohort study. International Journal of Cancer. 2017 Jul 15;141(2):279-286.
- Li B, Li X et al. Dichloroacetate and metformin synergistically suppress the growth of ovarian cancer cells. Oncotarget. 2016 Sep 13;7(37):59458-59470.
- Xintaropoulou C, Ward C et al. A comparative analysis of inhibitors of the glycolysis pathway in breast and ovarian cancer cell line models. Oncotarget. 2015 Sep 22;6(28):25677-95; Saed GM, Fletcher NM, Jiang ZL, Abu-Soud HM, Diamond MP. Dichloroacetate induces apoptosis of epithelial ovarian cancer cells through a mechanism involving modulation of oxidative stress. Reproductive Sciences. 2011 Dec;18(12):1253-61.
- Zhang Y, Guo G et al. A hybrid platinum drug dichloroacetate-platinum(II) overcomes cisplatin drug resistance through dual organelle targeting. Anticancer Drugs. 2015 Aug;26(7):698-705.
- Olszewski U, Poulsen TT et al. In vitro cytotoxicity of combinations of dichloroacetate with anticancer platinum compounds. Clinical Pharmacology. 2010;2:177-83.
- Donahue RN, McLaughlin PJ, Zagon IS. The opioid growth factor (OGF) and low dose naltrexone (LDN) suppress human ovarian cancer progression in mice. Gynecologic Oncology. 2011 Aug;122(2):382-8.
- Donahue RN, McLaughlin PJ, Zagon IS. Low-dose naltrexone suppresses ovarian cancer and exhibits enhanced inhibition in combination with cisplatin. Experimental Biology and Medicine (Maywood). 2011 Jul;236(7):883-95.
- Tomar V, Kukreti S, Prakash S, Madan J, Chandra R. Noscapine and its analogs as chemotherapeutic agent: current updates. Current Topics in Medicinal Chemistry. 2017;17(2):174-188.
- Zhou J, Gupta K et al. Paclitaxel-resistant human ovarian cancer cells undergo c-Jun NH2-terminal kinase-mediated apoptosis in response to noscapine. Journal of Biological Chemistry. 2002 Oct 18;277(42):39777-85.
- Shen W, Liang B, Yin J, Li X, Cheng J. Noscapine increases the sensitivity of drug-resistant ovarian cancer cell line SKOV3/DDP to cisplatin by regulating cell cycle and activating apoptotic pathways. Cell Biochemistry and Biophysics. 2015 May;72(1):203-13; Su W, Huang L et al. Noscapine sensitizes chemoresistant ovarian cancer cells to cisplatin through inhibition of HIF-1α. Cancer Letters. 2011 Jun 1;305(1):94-9.
- Martin LTP, Nachtigal MW et al. Bitter taste receptors are expressed in human epithelial ovarian and prostate cancers cells and noscapine stimulation impacts cell survival. Molecular and Cellular Biochemistry. 2018 Oct 22.
- Li Y, Zhou YF et al. Chinese expert consensus on cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal malignancies. World Journal of Gastroenterology. 2016 Aug 14;22(30):6906-16.
- Jewell A, McMahon M, Khabele D. Heated intraperitoneal chemotherapy in the management of advanced ovarian cancer. Cancers (Basel). 2018 Sep 1;10(9). pii: E296; van Driel WJ, Koole SN, Sonke GS. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. New England Journal of Medicine. 2018 Apr 5;378(14):1363-1364; Hotouras A, Desai D et al. Heated intraperitoneal chemotherapy (HIPEC) for patients with recurrent ovarian cancer: a systematic literature review. International Journal of Gynecological Cancer. 2016 May;26(4):661-70; Kireeva GS, Gafton GI et al. HIPEC in patients with primary advanced ovarian cancer: Is there a role? A systematic review of short- and long-term outcomes. Surgical Oncology. 2018 Jun;27(2):251-258; Chua TC, Robertson G et al. Intraoperative hyperthermic intraperitoneal chemotherapy after cytoreductive surgery in ovarian cancer peritoneal carcinomatosis: systematic review of current results. Journal of Cancer Research and Clinical Oncology. 2009 Dec;135(12):1637-45; Huo YR, Richards A, Liauw W, Morris DL. Hyperthermic intraperitoneal chemotherapy (HIPEC) and cytoreductive surgery (CRS) in ovarian cancer: a systematic review and meta-analysis. European Journal of Surgical Oncology. 2015 Dec;41(12):1578-89; Helm CW, Richard SD et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer: first report of the HYPER-O registry. International Journal of Gynecological Cancer. 2010 Jan;20(1):61-9; Di Giorgio A, Naticchioni E et al. Cytoreductive surgery (peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of diffuse peritoneal carcinomatosis from ovarian cancer. Cancer. 2008 Jul 15;113(2):315-25; Ryu KS, Kim JH et al. Effects of intraperitoneal hyperthermic chemotherapy in ovarian cancer. Gynecologic Oncology. 2004 Aug;94(2):325-32.
- Polom K, Roviello G et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for treatment of ovarian cancer. International Journal of Hyperthermia. 2016 May;32(3):298-310; Cascales-Campos P, Gil J, Feliciangeli E, Parrilla P. HIPEC in ovarian cancer: treatment of a new era or is it the end of the pipeline? Gynecologic Oncology. 2015 Nov;139(2):363-8.
- Kleef R, Kekic S, Ludwig N. Successful treatment of advanced ovarian cancer with thermochemotherapy and adjuvant immune therapy. Case Reports in Oncology. 2012 May;5(2):212-5; Douwes F, BogoviC J, Douwes O, Migeod F, Grote C. Whole-body hyperthermia in combination with platinum-containing drugs in patients with recurrent ovarian cancer. International Journal of Clinical Oncology. 2004 Apr;9(2):85-91; Atmaca A, Al-Batran SE et al. Whole-body hyperthermia (WBH) in combination with carboplatin in patients with recurrent ovarian cancer—a phase II study. Gynecologic Oncology. 2009 Feb;112(2):384-8; Westermann AM, Grosen EA et al. A pilot study of whole body hyperthermia and carboplatin in platinum-resistant ovarian cancer. European Journal of Cancer. 2001 Jun;37(9):1111-7; Robins HI, Cohen JD, Schmitt CL Phase I clinical trial of carboplatin and 41.8 degrees C whole-body hyperthermia in cancer patients. Journal of Clinical Oncology. 1993 Sep;11(9):1787-94; Cohen JD, Robins HI. Whole body hyperthermia and intraperitoneal carboplatin in residual ovarian cancer. Advances in Experimental Medicine and Biology. 1990;267:197-202; Robins HI, Longo WL et al. Phase I trial of lonidamine with whole body hyperthermia in advanced cancer. Cancer Research. 1988 Nov 15;48(22):6587-92.
- Lemanne D, Maizes V. Advising women undergoing treatment for breast cancer: a narrative review. Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):902-909; Lindau ST, Abramsohn EM et al. Physical examination of the female cancer patient with sexual concerns: what oncologists and patients should expect from consultation with a specialist. CA: a Cancer Journal for Clinicians. 2016 May;66(3):241-63.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10): 882.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10): 882.
- Macciò A, Madeddu C et al. A randomized phase III clinical trial of a combined treatment for cachexia in patients with gynecological cancers: evaluating the impact on metabolic and inflammatory profiles and quality of life. Gynecologic Oncology. 2012 Mar;124(3):417-25.
- Pulsed low-dose pelvic reirradiation safe, provided tangible benefit for patients with few other options. Fox Chase Cancer Center, September 22, 2020. Viewed September 30, 2020; Paly JJ, Deng M et al. Pelvic reirradiation utilizing pulsed low-dose rate radiation therapy. American Journal of Clinical Oncology. 2020 Oct;43(10):748-751.
- Panahi Y, Saadat A, Beiraghdar F, Sahebkar A. Adjuvant therapy with bioavailability-boosted curcuminoids suppresses systemic inflammation and improves quality of life in patients with solid tumors: a randomized double-blind placebo-controlled trial. Phytotherapy Research. 2014 Oct;28(10):1461-7.
- Marx W, Ried K et al. Ginger—mechanism of action in chemotherapy-induced nausea and vomiting: a review. Critical Reviews in Food Science and Nutrition. 2017 Jan 2;57(1):141-146; Sheikhi MA, Ebadi A, Talaeizadeh A, Rahmani H. Alternative methods to treat nausea and v—omiting from cancer chemotherapy. Chemotherapy Research and Practice. 2015;2015:818759; Marx W, Kiss N, Isenring L. Is ginger beneficial for nausea and vomiting? An update of the literature. Current Opinion in Supportive and Palliative Care. 2015 Jun;9(2):189-95; Marx WM, Teleni L et al. Ginger (Zingiber officinale) and chemotherapy-induced nausea and vomiting: a systematic literature review. Nutrition Reviews. 2013 Apr;71(4):245-54; Lee J, Oh H. Ginger as an antiemetic modality for chemotherapy-induced nausea and vomiting: a systematic review and meta-analysis. Oncology Nursing Forum. 2013 Mar;40(2):163-70.
- Sontakke S, Thawani V, Naik MS. Ginger as an antiemetic in nausea and vomiting induced by chemotherapy: a randomized, cross-over, double blind study. Indian Journal of Pharmacology. 2003;35(1):32–36.
- Sanaati F, Najafi S, Kashaninia Z, Sadeghi M. Effect of ginger and chamomile on nausea and vomiting caused by chemotherapy in Iranian women with breast cancer. Asian Pacific Journal of Cancer Prevention. 2016;17(8):4125-9; Arslan M, Ozdemir L. Oral intake of ginger for chemotherapy-induced nausea and vomiting among women with breast cancer. Clinical Journal of Oncology Nursing. 2015 Oct;19(5):E92-7.
- Kim HS, Kim MK et al. Effect of red ginseng on genotoxicity and health-related quality of life after adjuvant chemotherapy in patients with epithelial ovarian cancer: a randomized, double blind, placebo-controlled trial. Nutrients. 2017 Jul 19;9(7). pii: E772.
- Yennurajalingam S, Tannir NM et al. A double-blind, randomized, placebo-controlled trial of Panax ginseng for cancer-related fatigue in patients with advanced cancer. Journal of the National Comprehensive Cancer Network. 2017 Sep;15(9):1111-1120.
- Arring NM, Millstine D, Marks LA, Nail LM. Ginseng as a treatment for fatigue: a systematic review. Journal of Alternative and Complementary Medicine. 2018 Jul;24(7):624-633.
- Chen MH, May BH, Zhou IW, Zhang AL, Xue CC. Integrative medicine for relief of nausea and vomiting in the treatment of colorectal cancer using oxaliplatin-based chemotherapy: a systematic review and meta-analysis. Phytotherapy Research. 2016 May;30(5):741-53.
- Brami C, Bao T, Deng G. Natural products and complementary therapies for chemotherapy-induced peripheral neuropathy: a systematic review. Critical Reviews in Oncology/Hematology. 2016 Feb;98:325-34; Mondal S, Choudhury KB, Sharma S, Gupta A, DuttaS. Comparative study among glutamine, acetyl-L-carnitine, vitamin-E and methylcobalamine for treatment of paclitaxel-induced peripheral neuropathy. Clinical Cancer Investigation Journal. 2014;3(3):213-219; Argyriou AA, Chroni E et al. Vitamin E for prophylaxis against chemotherapy-induced neuropathy: a randomized controlled trial. Neurology. 2005 Jan 11;64(1):26-31; Pace A, Savarese A et al. Neuroprotective effect of vitamin E supplementation in patients treated with cisplatin chemotherapy. Journal of Clinical Oncology. 2003 Mar 1;21(5):927-31.
- Abrams DI. The therapeutic effects of cannabis and cannabinoids: an update from the National Academies of Sciences, Engineering and Medicine report. European Journal of Internal Medicine. 2018 Mar;49:7-11.
- Mücke M, Weier M. Systematic review and meta-analysis of cannabinoids in palliative medicine. Journal of Cachexia, Sarcopenia and Muscle. 2018 Feb 5.
- Ahn WS, Kim DJ et al. Natural killer cell activity and quality of life were improved by consumption of a mushroom extract, Agaricus blazei Murill Kyowa, in gynecological cancer patients undergoing chemotherapy. International Journal of Gynecological Cancer. 2004 Jul-Aug;14(4):589-94.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Poole J. Individualised homeopathy after cancer treatment. Nursing Times. 2014 Oct 8-14;110(41):17-9.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Pelzer F, Tröger W, Nat DR. Complementary treatment with mistletoe extracts during chemotherapy: safety, neutropenia, fever, and quality of life assessed in a randomized study. Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):954-961.
- Freuding M, Keinki C et al. Mistletoe in oncological treatment: a systematic review: part 2: quality of life and toxicity of cancer treatment. Journal of Cancer Research and Clinical Oncology. 2019 Jan 23.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Hao J, Zhu X, Bensoussan A. Effects of nonpharmacological interventions in chemotherapy-induced peripheral neuropathy: an overview of systematic reviews and meta-analyses. Integrative Cancer Therapies. Jan-Dec 2020;19:1534735420945027; Noh H, Yoon SW, Park B. A systematic review of herbal medicine for chemotherapy-induced peripheral neuropathy (CIPN). Evidence Based Complementary and Alternative Medicine. 2018 Feb 14;2018:6194184; Wei X, Zhu L, Wang H, Wang C, Deng Q, Li X. Efficacy of traditional Chinese medicines in preventing oxaliplatin-induced peripheral neurotoxicity in cancer patients: a network meta-analysis. Chinese Herb Med. 2017;9(2):161-168; Deng B, Jia L, Cheng Z. Radix astragali-based Chinese herbal medicine for oxaliplatin-induced peripheral neuropathy: a systematic review and meta-analysis. Evidence-based Complementary and Alternative Medicine. 2016;2016:2421876.
- Sieja K, Talerczyk M. Selenium as an element in the treatment of ovarian cancer in women receiving chemotherapy. Gynecologic Oncology. 2004 May;93(2):320-7.
- Dias MA, Sampaio AL, Venosa AR, Meneses Ede A, Oliveira CA. The chemopreventive effect of Ginkgo biloba extract 761 against cisplatin ototoxicity: a pilot study. International Tinnitus Journal. 2015;19(2):12-9; Aydin D, Peker EG et al. Effects of Ginkgo biloba extract on brain oxidative condition after cisplatin exposure. Clinical and Investigative Medicine. 2016 Dec 1;39(6):27511.
- Etheridge AS, Kroll DJ, Mathews JM. Inhibition of paclitaxel metabolism in vitro in human hepatocytes by Ginkgo biloba preparations. Journal of Dietary Supplements. 2009;6(2):104-10.
- Agbabiaka TB, Wider B, Watson LK, Goodman C. Concurrent use of prescription drugs and herbal medicinal products in older adults: a systematic review. Drugs & Aging. 2017 Dec;34(12):891-905.
- Mei N, Guo X et al. Review of Ginkgo biloba-induced toxicity, from experimental studies to human case reports. Journal of Environmental Science and Health. Part C, Environmental Carcinogenisis and Ecotoxicology Reviews. 2017 Jan 2;35(1):1-28.
- Nunes SC, Serpa J. Glutathione in ovarian cancer: a double-edged sword. International Journal of Molecular Sciences. 2018 Jun 26;19(7). pii: E1882; Smyth JF, Bowman A, Perren T et al. Glutathione reduces the toxicity and improves quality of life of women diagnosed with ovarian cancer treated with cisplatin: results of a double-blind, randomised trial. Annals of Oncology. 1997;8(6):569-573.
- Leal AD, Qin R et al. North Central Cancer Treatment Group/Alliance trial N08CA-the use of glutathione for prevention of paclitaxel/carboplatin-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled study. Cancer. 2014 Jun 15;120(12):1890-7.
- Bogliun G, Marzorati L et al. Neurotoxicity of cisplatin +/- reduced glutathione in the first-line treatment of advanced ovarian cancer. International Journal of Gynecological Cancer. 1996;6:415-419.
- Colombo N, Bini S. et al. Weekly cisplatin and glutathione in relapsed ovarian carcinoma. International Journal of Gynecological Cancer. 1995;5:81-86.
- Ma Y, Chapman J et al. High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Science Translational Medicine. 2014 Feb 5;6(222):222ra18.
- Loven D, Levavi H et al. Long-term glutamate supplementation failed to protect against peripheral neurotoxicity of paclitaxel. European Journal of Cancer Care (Engl). 2009 Jan;18(1):78-83.
- Kim HS, Kim MK et al. Effect of red ginseng on genotoxicity and health-related quality of life after adjuvant chemotherapy in patients with epithelial ovarian cancer: a randomized, double blind, placebo-controlled trial. Nutrients. 2017 Jul 19;9(7). pii: E772.
- Sieja K, Talerczyk M. Selenium as an element in the treatment of ovarian cancer in women receiving chemotherapy. Gynecologic Oncology. 2004 May;93(2):320-7.
- Muecke R, Micke O et al. Impact of treatment planning target volumen (PTV) size on radiation induced diarrhoea following selenium supplementation in gynecologic radiation oncology--a subgroup analysis of a multicenter, phase III trial. Radiation Oncology. 2013 Mar 25;8:72.
- Muecke R, Micke O et al. Selenium in radiation oncology—15 years of experiences in Germany. Nutrients. 2018 Apr 13;10(4). pii: E483.
- Sánchez-González PD, López-Hernández FJ et al. Differential effect of quercetin on cisplatin-induced toxicity in kidney and tumor tissues. Food and Chemical Toxicology. 2017 Sep;107(Pt A):226-236.
- Rezk YA, Balulad SS, Keller RS, Bennett JA. Use of resveratrol to improve the effectiveness of cisplatin and doxorubicin: study in human gynecologic cancer cell lines and in rodent heart. American Journal of Obstetrics and Gynecology. 2006 May;194(5):e23-6.
- Donahue RN, McLaughlin PJ, Zagon IS. Low-dose naltrexone suppresses ovarian cancer and exhibits enhanced inhibition in combination with cisplatin. Experimental Biology and Medicine (Maywood). 2011 Jul;236(7):883-95.
- Mao-Ying QL, Kavelaars A et al. The anti-diabetic drug metformin protects against chemotherapy-induced peripheral neuropathy in a mouse model. PLoS One. 2014 Jun 23;9(6):e10070; Zhou W, Kavelaars A, Heijnen CJ. Metformin prevents cisplatin-induced cognitive impairment and brain damage in mice. PLoS One. 2016 Mar 28;11(3):e0151890.
- Zhou W, Kavelaars A, Heijnen CJ. Metformin prevents cisplatin-induced cognitive impairment and brain damage in mice. PLoS One. 2016 Mar 28;11(3):e0151890.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecol Oncol. 2011 Nov;123(2):346-50.
- Bober SL, Recklitis CJ, Michaud AL, Wright AA. Improvement in sexual function after ovarian cancer: effects of sexual therapy and rehabilitation after treatment for ovarian cancer. Cancer. 2018 Jan 1;124(1):176-182.
- Petersen RW, Quinlivan JA. Preventing anxiety and depression in gynaecological cancer: a randomised controlled trial.BJOG. 2002 Apr;109(4):386-94.
- Goerling U, Jaeger C et al. The efficacy of short-term psycho-oncological interventions for women with gynaecological cancer: a randomized study. Oncology. 2014;87(2):114-24.
- Spiegel D. The use of hypnosis in controlling cancer pain. CA: A Cancer Journal for Clinicians. 1985 Jul-Aug;35(4):221-31.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Danhauer SC, Tooze JA et al. Restorative yoga for women with ovarian or breast cancer: findings from a pilot study. Journal of the Society for Integrative Oncology. 2008 Spring;6(2):47-58.
- Lu W, Matulonis UA et al. The feasibility and effects of acupuncture on quality of life scores during chemotherapy in ovarian cancer: results from a pilot, randomized sham-controlled trial. Medical Acupuncture. 2012 Dec;24(4):233-240.
- Rithirangsriroj K, Manchana T, Akkayagorn L. Efficacy of acupuncture in prevention of delayed chemotherapy induced nausea and vomiting in gynecologic cancer patients. Gynecologic Oncology. 2015 Jan;136(1):82-6.
- Liu YQ, Sun S et al. Wrist-ankle acupuncture and ginger moxibustion for preventing gastrointestinal reactions to chemotherapy: a randomized controlled trial. Chinese Journal of Integrative Medicine. 2015 Sep;21(9):697-702.
- Paice JA, Portenoy R et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology. 2016 Sep 20;34(27):3325-45.
- CancerNet. Peripheral Neuropathy. American Society of Clinical Oncology. May 2017. Viewed March 14, 2018.
- Gross AH, Cromwell J, Fonteyn M, Matulonis UA, Hayman LL. Hopelessness and complementary therapy use in patients with ovarian cancer. Cancer Nursing. 2013 Jul-Aug;36(4):256-64.
- Donoyama N, Satoh T, Hamano T, Ohkoshi N, Onuki M. Physical effects of Anma therapy (Japanese massage) for gynecologic cancer survivors: a randomized controlled trial. Gynecologic Oncology. 2016 Sep;142(3):531-8.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Greenlee H, DuPont-Reyes MJ et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA A Cancer Journal for Clinicians. 2017 May 6;67(3):194-232.
- Bauersfeld SP, Kessler CS et al. The effects of short-term fasting on quality of life and tolerance to chemotherapy in patients with breast and ovarian cancer: a randomized cross-over pilot study. BMC Cancer. 2018 Apr 27;18(1):476.
- Riedinger C, Kimball KJ et al. Water-only fasting and its effect on chemotherapy administration in gynecologic malignancies. Society of Gynecologic Oncology 20/20 Annual Meeting on Women's Cancer.
- Safdie FM, Dorff T et al. Fasting and cancer treatment in humans: a case series report. Aging (Milano) 2009;1:988–1007.
- Hisada Y, Mackman N. Cancer-associated pathways and biomarkers of venous thrombosis. Blood. 2017 Sep 28;130(13):1499-1506.
- Block KI. Life over Cancer: The Block Center Program for Integrative Cancer Treatment. New York: Bantam Dell. 2009. p. 368-390.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013; Dixon-Suen SC, Nagle CM et al. Adult height is associated with increased risk of ovarian cancer: a Mendelian randomisation study. British Journal of Cancer. 2018 Apr;118(8):1123-1129.
- Continuous Update Project. Ovarian cancer: how diet, nutrition and physical activity affect ovarian cancer risk. Diet and Cancer Report. World Cancer Research Fund International. Viewed January 31, 2019; Turck D; Comité de nutrition de la Société française de pédiatrie; Breast feeding: health benefits for child and mother]. [Article in French] Archives de Pediatrie. 2005 Dec;12 Suppl 3:S145-65; Foong KW, Bolton H. Obesity and ovarian cancer risk: a systematic review. Post Reproductive Health. 2017 Dec;23(4):183-198; La Vecchia C. Ovarian cancer: epidemiology and risk factors. European Journal of Cancer and Prevention. 2017 Jan;26(1):55-62; Harris HR, Rice MS et al. Lifestyle and reproductive factors and ovarian cancer risk by p53 and MAPK expression. Cancer Epidemiology, Biomarkers & Prevention. 2018 Jan;27(1):96-102.
- Dun A, Zhao X et al. Association between night-shift work and cancer risk: updated systematic review and meta-analysis. Frontiers in Oncology. 2020 Jun 23;10:1006.
- Carter BD, Diver WR, Hildebrand JS, Patel AV, Gapstur SM. Circadian disruption and fatal ovarian cancer. American Journal of Preventive Medicine. 2014 Mar;46(3 Suppl 1):S34-41; Poole EM, Schernhammer ES, Tworoger SS. Rotating night shift work and risk of ovarian cancer. Cancer Epidemiology, Biomarkers & Prevention. 2011 May;20(5):934-8.
- Nené NR, Reisel D et al. Association between the cervicovaginal microbiome, BRCA1 mutation status, and risk of ovarian cancer: a case-control study. Lancet Oncology. 2019 Aug;20(8):1171-1182.
- ASCO Post Staff. Study clarifies time-dependent effects of oral contraceptives on risk of ovarian, endometrial, and breast cancers. ASCO Post. December 23, 2020. Viewed January 5, 2021; Karlsson T, Johansson T, Höglund J, Ek WE, Johansson Å. Time-dependent effects of oral contraceptive use on breast, ovarian and endometrial cancers. Cancer Research. 2020 Dec 17:canres.2476.2020.
- Qu XL, Fang Y, Zhang M, Zhang YZ. Phytoestrogen intake and risk of ovarian cancer: a meta- analysis of 10 observational studies. Asian Pacific Journal of Cancer Prevention. 2014;15(21):9085-91; Bandera EV, King M et al. Phytoestrogen consumption from foods and supplements and epithelial ovarian cancer risk: a population-based case control study. BMC Womens Health. 2011 Sep 23;11:40..
- Sahin K, Yenice E et al. Genistein prevents development of spontaneous ovarian cancer and inhibits tumor growth in hen model. Cancer Prevention and Research (Philadelphia, PA). 2019 Jan 16.
- Terry PD, Qin B et al. Supplemental selenium may decrease ovarian cancer risk in African-American women. Journal of Nutrition. 2017 Apr;147(4):621-627.
- Fleischauer AT, Olson SH et al. Dietary antioxidants, supplements, and risk of epithelial ovarian cancer. Nutrition and Cancer. 2001;40(2):92-8.
- Thomson CA, Neuhouser ML et al. The role of antioxidants and vitamin A in ovarian cancer: results from the Women's Health Initiative. Nutrition and Cancer. 2008;60(6):710-9; Fairfield KM, Hankinson SE et al. Risk of ovarian carcinoma and consumption of vitamins A, C, and E and specific carotenoids: a prospective analysis. Cancer. 2001 Nov 1;92(9):2318-26.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Raymond YC, Glenda CS, Meng LK. Effects of high doses of vitamin C on cancer patients in Singapore: nine cases. Integrative Cancer Therapies. 2016;15(2):197-204.
- Drisko JA, Chapman J, Hunter VJ. The use of antioxidants with first-line chemotherapy in two cases of ovarian cancer. Journal of the American College of Nutrition. 2003 Apr;22(2):118-23.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Ye B, Aponte M et al. Ginkgo biloba and ovarian cancer prevention: epidemiological and biological evidence. Cancer Letters. 2007 Jun 18;251(1):43-52.
- Jiang W, Qiu W et al. Ginkgo may prevent genetic-associated ovarian cancer risk: multiple biomarkers and anticancer pathways induced by ginkgolide B in BRCA1-mutant ovarian epithelial cells. European Journal of Cancer Prevention. 2011 Nov;20(6):508-17.
- Agbabiaka TB, Wider B, Watson LK, Goodman C. Concurrent use of prescription drugs and herbal medicinal products in older adults: a systematic review. Drugs & Aging. 2017 Dec;34(12):891-905.
- Mei N, Guo X et al. Review of Ginkgo biloba-induced toxicity, from experimental studies to human case reports. Journal of Environmental Science and Health. Part C, Environmental Carcinogenisis and Ecotoxicology Reviews. 2017 Jan 2;35(1):1-28.
- Dikshit A, Hales K, Hales DB. Whole flaxseed diet alters estrogen metabolism to promote 2-methoxtestradiol-induced apoptosis in hen ovarian cancer. Journal of Nutritional Biochemistry. 2017 Apr;42:117-125.
- Sahin K, Yenice E et al. Lycopene protects against spontaneous ovarian cancer formation in laying hens. Journal of Cancer Prevention. 2018 Mar;23(1):25-36.
- Koushik A, Wang M et al. Intake of vitamins A, C, and E and folate and the risk of ovarian cancer in a pooled analysis of 10 cohort studies. Cancer Causes & Control. 2015 Sep;26(9):1315-27.
- Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA. Dietary intake and ovariancancer risk: a systematic review. Cancer Epidemiology, Biomarkers & Prevention.
- 2014 Feb;23(2):255-73.
- Qin B, Moorman PG et al. Dairy, calcium, vitamin D and ovarian cancer risk in African-American women. British Journal Cancer. 2016 Oct 25;115(9):1122-1130.
- Verdoodt F, Kjaer SK, Friis S. Influence of aspirin and non-aspirin NSAID use on ovarian and endometrial cancer: summary of epidemiologic evidence of cancer risk and prognosis. Maturitas. 2017 Jun;100:1-7; Zhang D, Bai B, Xi Y, Wang T, Zhao Y. Is aspirin use associated with a decreased risk of ovarian cancer? A systematic review and meta-analysis of observational studies with dose-response analysis. Gynecologic Oncology. 2016 Aug;142(2):368-77; Baandrup L, Faber MT et al. Nonsteroidal anti-inflammatory drugs and risk of ovarian cancer: systematic review and meta-analysis of observational studies. Acta Obstetricia et Gynecologica Scandinavica. 2013 Mar;92(3):245-55.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Khan MS, Fatima K, Rameez. Impact of statins on risk and survival of ovarian cancer. Journal of Gynecologic Oncology. 2015 Jul;26(3):240-1.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Panahi Y, Saadat A, Beiraghdar F, Sahebkar A. Adjuvant therapy with bioavailability-boosted curcuminoids suppresses systemic inflammation and improves quality of life in patients with solid tumors: a randomized double-blind placebo-controlled trial. Phytotherapy Research. 2014 Oct;28(10):1461-7.
- Ferguson LR, Chen H et al. Genomic instability in human cancer: molecular insights and opportunities for therapeutic attack and prevention through diet and nutrition. Seminars in Cancer Biology. 2015 Dec;35 Suppl:S5-S24.
- Chobotova K, Vernallis AB, Majid FA.Bromelain's activity and potential as an anti-cancer agent: current evidence and perspectives. Cancer Letters. 2010 Apr 28;290(2):148-56.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Chen X, Anderson JJ. Isoflavones inhibit proliferation of ovarian cancer cells in vitro via an estrogen receptor-dependent pathway. Nutrition and Cancer. 2001;41(1-2):165-71; Liu J, Viswanadhapalli S et al. Therapeutic utility of natural estrogen receptor beta agonists on ovarian cancer. Oncotarget. 2017 Jul 25;8(30):50002-50014.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Ahn WS, Kim DJ et al. Natural killer cell activity and quality of life were improved by consumption of a mushroom extract, Agaricus blazei Murill Kyowa, in gynecological cancer patients undergoing chemotherapy. International Journal of Gynecological Cancer. 2004 Jul-Aug;14(4):589-94.
- Mukai H, Watanabe T, Ando M, Katsumata N. An alternative medicine, Agaricus blazei, may have induced severe hepatic dysfunction in cancer patients. Japanese Journal of Clinical Oncology. 2006 Dec;36(12):808-10.
- Kikuchi Y, Kizawa I et al. Effects of PSK on interleukin-2 production by peripheral lymphocytes of patients with advanced ovarian carcinoma during chemotherapy. Japanese Journal of Cancer Research. 1988 Jan;79(1):125-30.
- Kikuchi Y, Kizawa I et al. [Effects of cimetidine and PSK on interleukin-2 production by PBL in patients with advanced ovarian carcinoma during the course of chemotherapy]. [Article in Japanese] Nihon Sanka Fujinka Gakkai Zasshi. 1987 Nov;39(11):1987-92.
- Ishii K, Kita T et al. [Antitumor effect of PSK and its combined effect with CDDP on ovarian serous adenocarcinoma-bearing nude mice]. [Article in Japanese] Nihon Sanka Fujinka Gakkai Zasshi. 1993 Apr;45(4):333-9.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Lu W, Matulonis UA et al. Acupuncture for chemotherapy-induced neutropenia in patients with gynecologic malignancies: a pilot randomized, sham-controlled clinical trial. Journal of Alternative and Complementary Medicine. 2009 Jul;15(7):745-53.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889.
- Nelson R. Can integrative oncology extend life in advanced disease? Medscape Medical News. October 25, 2013. Viewed February 1, 2019.
- Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Ovarian Cancer. Viewed February 8, 2019.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016. p. 316.
- Ben-Arye E, Schiff E, Steiner M, Keshet Y, Lavie O. Attitudes of patients with gynecological and breast cancer toward integration of complementary medicine in cancer care. International Journal of Gynecological Cancer. 2012;22(1):146‐153.
- Ben-Arye B. Integrative Gynecologic Oncology--would value your input [personal email communication with Laura Pole]. May 27, 2020.
- Shalom-Sharabi I, Lavie O, Samuels N, Keinan-Boker L, Lev E, Ben-Arye E. Can complementary medicine increase adherence to chemotherapy dosing protocol? A controlled study in an integrative oncology setting. Journal of Cancer Research and Clinical Oncology. 2017;143(12):2535‐2543.
- Shalom-Sharabi I, Samuels N et al. Impact of a complementary/integrative medicine program on the need for supportive cancer care-related medications. Supportive Care in Cancer. 2017;25(10):3181‐3190.
- Ben-Arye E, Samuels N et al. Quality-of-life outcomes in patients with gynecologic cancer referred to integrative oncology treatment during chemotherapy. Supportive Care in Cancer. 2015;23(12):3411‐3419.
- Shalom-Sharabi I, Samuels N et al. Effect of a patient-tailored integrative medicine program on gastro-intestinal concerns and quality of life in patients with breast and gynecologic cancer. Journal of Cancer Research and Clinical Oncology. 2017;143(7):1243‐1254.
- Ben-Arye E, Aharonson ML, Schiff E, Samuels N. Alleviating gastro-intestinal symptoms and concerns by integrating patient-tailored complementary medicine in supportive cancer care. Clinical Nutrition. 2015;34(6):1215‐1223.
- Shalom-Sharabi I, Samuels N et al. Effect of a patient-tailored integrative medicine program on gastro-intestinal concerns and quality of life in patients with breast and gynecologic cancer. Journal of Cancer Research and Clinical Oncology. 2017;143(7):1243‐1254; Ben-Arye E, Samuels N et al. Quality-of-life outcomes in patients with gynecologic cancer referred to integrative oncology treatment during chemotherapy. Supportive Care in Cancer. 2015;23(12):3411‐3419.
- Keshet Y, Schiff E, Samuels N, Ben-Arye E. Giving voice to cancer patients: assessing non-specific effects of an integrative oncology therapeutic program via short patient narratives. Psychooncology. 2015;24(2):169‐174.
- Ben-Arye E, Samuels N, Schiff E, Lavie O. Designing an integrative gynecologic oncology model of supportive care: call for a cross-cultural international collaboration. Supportive Care in Cancer. 2016;24(4):1457‐1458.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Block KI.Life over Cancer: The Block Center Program for Integrative Cancer Treatment. New York: Bantam Dell. 2009.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Chan KK, Yao TJ et al. The use of Chinese herbal medicine to improve quality of life in women undergoing chemotherapy for ovarian cancer: a double-blind placebo-controlled randomized trial with immunological monitoring. Annals of Oncology. 2011 Oct;22(10):2241-9.
- Bae K, Kim E, Choi JJ, Kim MK, Yoo HS. The effectiveness of anticancer traditional Korean medicine treatment on the survival in patients with lung, breast, gastric, colorectal, hepatic, uterine, or ovarian cancer: a prospective cohort study protocol. Medicine (Baltimore). 2018 Oct;97(41):e12444.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889; Playdon MC, Nagle CM et al. Pre-diagnosis diet and survival after a diagnosis of ovarian cancer. British Journal of Cancer. 2017 Jun 6;116(12):1627-1637; Webb PM, de Fazio A et al. Circulating 25-hydroxyvitamin D and survival in women with ovarian cancer. American Journal of Clinical Nutrition. 2015 Jul;102(1):109-14; Ong JS1,2, Cuellar-Partida G et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. International Journal of Epidemiology. 2016 Oct;45(5):1619-1630.
- Playdon MC, Nagle CM et al. Pre-diagnosis diet and survival after a diagnosis of ovarian cancer. British Journal of Cancer. 2017 Jun 6;116(12):1627-1637.
- Wax E, Zieve D. Facts about polyunsaturated fats. Medline Plus. April 30, 2019. Viewed May 7, 2019.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889; Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA. Dietary intake and ovarian cancer risk: a systematic review. Cancer Epidemiology, Biomarkers & Prevention. 2014 Feb;23(2):255-73; Xu H1, Ding Y, Xin X, Wang W, Zhang D. Dietary fiber intake is associated with a reduced risk of ovarian cancer: a dose-response meta-analysis. Nutrition Research. 2018 Sep;57:1-11; Schwab U, Lauritzen L et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food & Nutrition Research. 2014 Jul 10;58; Qiu W, Lu H, Qi Y, Wang X. Dietary fat intake and ovarian cancer risk: a meta-analysis of epidemiological studies. Oncotarget. 2016 Jun 14;7(24):37390-37406; Ganmaa D, Sato A. The possible role of female sex hormones in milk from pregnant cows in the development of breast, ovarian and corpus uteri cancers. Medical Hypotheses. 2005;65(6):1028-37; Larsson SC, Wolk A. Tea consumption and ovarian cancer risk in a population-based cohort. Archives of Internal Medicine. 2005 Dec 12-26;165(22):2683-6; Larsson SC, Giovannucci E, Wolk A. Dietary folate intake and incidence of ovarian cancer: the Swedish Mammography Cohort. Journal of the National Cancer Institute. 2004 Mar 3;96(5):396-402; Silvera SA, Jain M, Howe GR, Miller AB, Rohan TE. Carotenoid, vitamin A, vitamin C, and vitamin E intake and risk of ovarian cancer: a prospective cohort study. Cancer Epidemiology, Biomarkers & Prevention. 2006 Feb;15(2):395-7; Lee AH, Su D et al. Soy and isoflavone intake associated with reduced risk of ovarian cancer in southern Chinese women. Nutrition Research. 2014 Apr;34(4):302-7; Qu XL, Fang Y, Zhang M, Zhang YZ. Phytoestrogen intake and risk of ovarian cancer: a meta- analysis of 10 observational studies. Asian Pacific Journal of Cancer Prevention. 2014;15(21):9085-91; Myung SK, Ju W, Choi HJ, Kim SC; Korean Meta-Analysis (KORMA) Study Group. Soy intake and risk of endocrine-related gynaecological cancer: a meta-analysis. BJOG. 2009 Dec;116(13):1697-705; Tung KH, Wilkens LR et al. Association of dietary vitamin A, carotenoids, and other antioxidants with the risk of ovarian cancer. Cancer Epidemiology, Biomarkers & Prevention. 2005 Mar;14(3):669-76; Jeong NH, Song ES et al. Plasma carotenoids, retinol and tocopherol levels and the risk of ovarian cancer. Acta Obstet Gynecol Scand. 2009;88(4):457-62; Li X, Xu J. Meta-analysis of the association between dietary lycopene intake and ovarian cancer risk in postmenopausal women. Scientific Reports. 2014 May 9;4:4885; Tang L, Lee AH, Su D, Binns CW. Fruit and vegetable consumption associated with reduced risk of epithelial ovarian cancer in southern Chinese women. Gynecologic Oncology. 2014 Jan;132(1):241-7; Gifkins D, Olson SH et al. Total and individual antioxidant intake and risk of epithelial ovarian cancer. BMC Cancer. 2012 Jun 1;12:211; Merritt MA, Cramer DW et al. Dietary fat intake and risk of epithelial ovarian cancer by tumour histology. British Journal of Cancer. 2014 Mar 4;110(5):1392-401; Hoang T, Myung SK, Pham TT. Dietary intake of omega-3 fatty acids and endocrine-related gynecological cancer: a meta-analysis of observational studies. Cancer Research and Treatment. 2018 Oct 17; Leung AC1, Cook LS et al. Tea, coffee, and caffeinated beverage consumption and risk of epithelial ovarian cancers. Cancer Epidemiology. 2016 Dec;45:119-125; Hashibe M, Galeone C et al. Coffee, tea, caffeine intake, and the risk of cancer in the PLCO cohort. British Journal of Cancer. 2015 Sep 1;113(5):809-16.
- Trudel D, Labbé DP et al. A two-stage, single-arm, phase II study of EGCG-enriched green tea drink as a maintenance therapy in women with advanced stage ovarian cancer. Gynecologic Oncology. 2013 Nov;131(2):357-61.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889.
- Tabung FK, Huang T et al. The inflammatory potential of diet and ovarian cancer risk: results from two prospective cohort studies. British Journal of Cancer. 2017 Sep 5;117(6):907-911.
- Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA. Dietary intake and ovarian cancer risk: a systematic review. Cancer Epidemiology, Biomarkers & Prevention. 2014 Feb;23(2):255-73; Keum N, Lee DH et al. Egg intake and cancers of the breast, ovary and prostate: a dose-response meta-analysis of prospective observational studies. British Journal of Nutrition. 2015 Oct 14;114(7):1099-107; Thorning TK, Raben A et al. Milk and dairy products: good or bad for human health? An assessment of the totality of scientific evidence. Food & Nutrition Research. 2016 Nov 22;60:32527; Cancer Epidemiol Biomarkers Prev. 2006 Feb;15(2):395-7; Silvera SA, Jain M, Howe GR, Miller AB, Rohan TE. Carotenoid, vitamin A, vitamin C, and vitamin E intake and risk of ovarian cancer: a prospective cohort study. Cancer Epidemiology, Biomarkers & Prevention. 2006 Feb;15(2):395-7; Jolfaie NR, Rouhani MH, Onvani S, Azadbakht L. The association between vitamin D and health outcomes in women: a review on the related evidence. Journal of Research in Medical Sciences. 2016 Sep 1;21:76. eCollection 2016; Tschernichovsky R, Goodman A et al. Risk-reducing strategies for ovarian cancer in BRCA mutation carriers: a balancing act. Oncologist. 2017 Apr;22(4):450-459; Hashibe M, Galeone C et al. Coffee, tea, caffeine intake, and the risk of cancer in the PLCO cohort. British Journal of Cancer. 2015 Sep 1;113(5):809-16.
- Qu XL, Fang Y, Zhang M, Zhang YZ. Phytoestrogen intake and risk of ovarian cancer: a meta- analysis of 10 observational studies. Asian Pacific Journal of Cancer Prevention. 2014;15(21):9085-91.
- Mulholland HG, Murray LJ, Cardwell CR, Cantwell MM. Dietary glycaemic index, glycaemic load and endometrial and ovarian cancer risk: a systematic review and meta-analysis. British Journal of Cancer. 2008 Aug 5;99(3):434-41.
- Zhang Y, Wu J et al. Association of serum lipids and severity of epithelial ovarian cancer: an observational cohort study of 349 Chinese patients. Journal of Biomedical Research. 2018 Sep 29;32(5):336-342.
- Schofield C, Newton RU, Galvão DA, Cohen PA, Peddle-McIntyre CJ. A physiological profile of ovarian cancer survivors to inform tailored exercise interventions and the development of exercise oncology guidelines. International Journal of Gynecologic Cancer. 2017 Sep;27(7):1560-1567.
- Poole EM, Konstantinopoulos PA, Terry KL. Prognostic implications of reproductive and lifestyle factors in ovarian cancer. Gynecologic Oncology. 2016 Sep;142(3):574-87.
- von Gruenigen VE, Frasure HE et al. Feasibility of a lifestyle intervention for ovarian cancer patients receiving adjuvant chemotherapy. Gynecologic Oncology. 2011 Aug;122(2):328-33.
- Zhang Q, Li F, Zhang H, Yu X, Cong Y. Effects of nurse-led home-based exercise & cognitive behavioral therapy on reducing cancer-related fatigue in patients with ovarian cancer during and after chemotherapy: A randomized controlled trial. International Journal of Nursing Studies. 2018 Feb;78:52-60.
- Crawford JJ, Vallance JK, Holt NL, Courneya KS. Associations between exercise and posttraumatic growth in gynecologic cancer survivors.Supportive Care in Cancer. 2015 Mar;23(3):705-14.
- Smits A, Lopes A et al. The effect of lifestyle interventions on the quality of life of gynaecological cancer survivors: a systematic review and meta-analysis. Gynecologic Oncology. 2015 Dec;139(3):546-52.
- Yeganeh L, Harrison C, Vincent AJ, Teede H, Boyle JA. Effects of lifestyle modification on cancer recurrence, overall survival and quality of life in gynaecological cancer survivors: a systematic review and meta-analysis. Maturitas. 2018 May;111:82-89.
- Beavis AL, Smith AJ, Fader AN. Lifestyle changes and the risk of developing endometrial and ovarian cancers: opportunities for prevention and management. International Journal of Women’s Health. 2016 May 23;8:151-67.
- Fashler SR, Weinrib AZ, Azam MA, Katz J. The use of Acceptance and Commitment Therapy in oncology settings: a narrative review. Psychological Reports. 2018 Apr;121(2):229-252.
- Roberts AL, Huang T et al. Posttraumatic stress disorder (PTSD) is associated with increased risk of ovarian cancer: a prospective and retrospective longitudinal cohort study. Cancer Research. 2019 Sep 5. pii: canres.1222.2019.
- Thaker PH, Lutgendorf SK, Sood AK. The neuroendocrine impact of chronic stress on cancer. Cell Cycle. 2007 Feb 15;6(4):430-3.
- Crane TE, Skiba MB, Donzella S, Thomson CA, Parthasarathy S. 0414 chronotype and sleep among ovarian cancer survivors participating in a lifestyle intervention. Sleep. 2020 April ;43(Supplement_1):A158–A159.
- Hurley S, Goldberg D, Bernstein L, Reynolds P. Sleep duration and cancer risk in women. Cancer Causes & Control. 2015 Jul;26(7):1037-45.
- Penninkilampi R, Eslick GD. Perineal talc use and ovarian cancer: a systematic review and meta-analysis. Epidemiology. 2018 Jan;29(1):41-49.
- Park SH, Kim KY et al. Cell growth of ovarian cancer cells is stimulated by xenoestrogens through an estrogen-dependent pathway, but their stimulation of cell growth appears not to be involved in the activation of the mitogen-activated protein kinases ERK-1 and p38. Journal of Reproduction and Development. 2009 Feb;55(1):23-9.
- Janssen S, Solomon G, Schettler T. Toxicant and Disease Database. Ovarian cancer. Collaborative on Health and the Environment. 2011. Viewed February 3, 2019.
- Janssen S, Solomon G, Schettler T. Toxicant and Disease Database. Ovarian cancer. Collaborative on Health and the Environment. 2011. Viewed February 3, 2019.
- Hill EM, Watkins K et al. Women with ovarian cancer: examining the role of social support and rumination in posttraumatic growth, psychological distress, and psychological well-being. Journal of Clinical Psychology in Medical Settings. 2017 Mar;24(1):47-58.
- Wen Q, Shao Z et al. Mental distress, quality of life and social support in recurrent ovarian cancer patients during active chemotherapy. European Journal of Obstetrics, Gynecology and Reproductive Biology. 2017 Sep;216:85-91.
- Lutgendorf SK, Sood AK et al. Social support, psychological distress, and natural killer cell activity in ovarian cancer. Journal of Clinical Oncology. 2005 Oct 1;23(28):7105-13.
- Idahl A, Hermansson A, Lalos A. Social support and ovarian cancer incidence—a Swedish prospective population-based study. Gynecologic Oncology. 2018 May;149(2):324-328.
- de Moor JS, de Moor CA et al. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosomatic Medicine. 2006 Jul-Aug;68(4):555-62.
- de Moor JS, de Moor CA et al. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosomatic Medicine. 2006 Jul-Aug;68(4):555-62.
- National Comprehensive Cancer Network: Ovarian Cancer: Professional Guidelines (login required). Viewed February 27, 2019.
- Block KI. Life over Cancer: The Block Center Program for Integrative Cancer Treatment. New York: Bantam Dell. 2009. p. 482.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):881-889.
- Alyami M, Hübner M et al. Pressurised intraperitoneal aerosol chemotherapy: rationale, evidence, and potential indications. Lancet Oncology. 2019 Jul;20(7):e368-e377.
- Pulsed low-dose pelvic reirradiation safe, provided tangible benefit for patients with few other options. Fox Chase Cancer Center, September 22, 2020. Viewed September 30, 2020; Paly JJ, Deng M et al. Pelvic reirradiation utilizing pulsed low-dose rate radiation therapy. American Journal of Clinical Oncology. 2020 Oct;43(10):748-751.
- Percutaneous Thermal Ablation. NorthShore University HealthSystem. Viewed April 22, 2021.
- Yuan F, Wei SH et al. Image-guided percutaneous thermal ablation of oligometastatic ovarian and non-ovarian gynecologic tumors. Journal of Vascular and Interventional Radiology. 2021 Feb 16:S1051-0443(21)00315-8.
- Lin L, Liu C et al. Anaesthetic technique may affect prognosis for ovarian serous adenocarcinoma: a retrospective analysis. British Journal of Anaesthesia. 2011 Jun;106(6):814-22.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10): 882.
- Kiselev VI, Ashrafyan LA et al. A new promising way of maintenance therapy in advanced ovarian cancer: a comparative clinical study. BMC Cancer. 2018 Sep 20;18(1):904.
- Chuffa LGA, Reiter RJ, Lupi LA. Melatonin as a promising agent to treat ovarian cancer: molecular mechanisms. Carcinogenesis. 2017 Oct 1;38(10):945-952; de Almeida Chuffa LG, Seiva FRF et al. Mitochondrial functions and melatonin: a tour of the reproductive cancers. Cellular and Molecular Life Sciences. 2018 Nov 14.
- Kim JH, Jeong SJ et al. Melatonin synergistically enhances cisplatin-induced apoptosis via the dephosphorylation of ERK/p90 ribosomal S6 kinase/heat shock protein 27 in SK-OV-3 cells. Journal of Pineal Research. 2012 Mar;52(2):244-52; Lissoni P, Paolorossi F et al. A phase II study of tamoxifen plus melatonin in metastatic solid tumour patients. British Journal of Cancer. 1996 Nov;74(9):1466-8.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Freuding M, Keinki C, Micke O, Buentzel J, Huebner J. Mistletoe in oncological treatment: a systematic review: part 1:survival and safety. Journal of Cancer Research and Clinical Oncology. 2019 Jan 23.
- Grossarth-Maticek R, Ziegler R. Prospective controlled cohort studies on long-term therapy of ovarian cancer patients with mistletoe (Viscum album L.) extracts Iscador. Arzneimittelforschung. 2007;57(10):665-78.
- Kienle GS, Glockmann A, Schink M, Kiene H. Viscum album L. extracts in breast and gynaecological cancers: a systematic review of clinical and preclinical research. Journal of Experimental and Clinical Cancer Research. 2009 Jun 11;28:79.
- Ben-Arye E, Lavie O. Safety of herbal medicine use during chemotherapy in patients with ovarian cancer: a "bedside-to-bench" approach. Med Oncol. 2017 Apr;34(4):54.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Fujimoto K, Tomonaga M, Goto S. A case of recurrent ovarian cancer successfully treated with adoptive immunotherapy and lentinan. Anticancer Research. 2006 Nov-Dec;26(6A):4015-8.
- Shimizu Y, Hasumi K et al. [Successful treatment of a patient with recurrent ovarian cancer by lentinan combined with intraarterial 5FU]. [Article in Japanese] Nihon Gan Chiryo Gakkai Shi. 1989 Mar 20;24(3):647-51.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Schwartz L, Buhler L, Icard P, Lincet H, Steyaert JM. Metabolic treatment of cancer: intermediate results of a prospective case series. Anticancer Research. 2014 Feb;34(2):973-80.
- Drisko JA, Chapman J, Hunter VJ. The use of antioxidants with first-line chemotherapy in two cases of ovarian cancer. Journal of the American College of Nutrition. 2003 Apr;22(2):118-23.
- Bohm S, Oriana S et al. Dose intensification of platinum compounds with glutathione protection as induction chemotherapy for advanced ovarian carcinoma, Oncology 1999; 57(2):115-120.
- Nunes SC, Serpa J. Glutathione in ovarian cancer: a double-edged sword. International Journal of Molecular Sciences. 2018 Jun 26;19(7). pii: E1882.
- Nauman G, Gray JC, Parkinson R, Levine M, Paller CJ. Systematic review of intravenous ascorbate in cancer clinical trials. Antioxidants (Basel). 2018 Jul 12;7(7):89.
- Ma Y, Chapman J et al. High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Science Translational Medicine. 2014 Feb 5;6(222):222ra18.
- Chen Q, Espey MG et al. Pharmacologic doses of ascorbate act as a prooxidant and decrease growth of aggressive tumor xenografts in mice. Proceedings of the National Academy of Sciences U S A. 2008 Aug 12;105(32):11105-9.
- Kobayashi H, Yoshida R et al. Suppressing effects of daily oral supplementation of beta-glucan extracted from Agaricus blazei Murill on spontaneous and peritoneal disseminated metastasis in mouse model. Journal of Cancer Research and Clinical Oncology. 2005 Aug;131(8):527-38.
- Mukai H, Watanabe T, Ando M, Katsumata N. An alternative medicine, Agaricus blazei, may have induced severe hepatic dysfunction in cancer patients. Japanese Journal of Clinical Oncology. 2006 Dec;36(12):808-10.
- Kakar SS, Ratajczak MZ et al. Withaferin a alone and in combination with cisplatin suppresses growth and metastasis of ovarian cancer by targeting putative cancer stem cells. PLoS One. 2014 Sep 29;9(9):e107596.
- Chu Z, Wang Z, Liu T, Xiong S, Liu B. Evaluation of the effects of astragalus membranaceus on the pharmacokinetics of pemetrexed disodium and gemcitabine in rats by a simple high-performance liquid chromatography/UV method. Journal of Analytical Methods in Chemistry. 2019 Apr 28;2019:3162426.
- Yin G, Tang D et al. Combination efficacy of Astragalus membranaceus and Curcuma wenyujin at different stages of tumor progression in an imageable orthotopic nude mouse model of metastatic human ovarian cancer expressing red fluorescent protein
- Zhao J, Pan Y et al. Dihydroartemisinin and curcumin synergistically induce apoptosis in SKOV3 cells via upregulation of MiR-124 targeting midkine. Cell Physiology and Biochemistry. 2017;43(2):589-601.
- Dikshit A, Hales K, Hales DB. Whole flaxseed diet alters estrogen metabolism to promote 2-methoxtestradiol-induced apoptosis in hen ovarian cancer. Journal of Nutritional Biochemistry. 2017 Apr;42:117-125.
- Holzapfel NP, Shokoohmand A et al. Lycopene reduces ovarian tumor growth and intraperitoneal metastatic load. American Journal of Cancer Research. 2017 Jun 1;7(6):1322-1336. eCollection 2017.
- Cho HJ, Suh DS et al. Silibinin inhibits tumor growth through downregulation of extracellular signal-regulated kinase and Akt in vitro and in vivo in human ovarian cancer cells. Journal of Agricultural and Food Chemistry. 2013 May 1;61(17):4089-96.
- Pashaei-Asl F, Pashaei-Asl R et al. Enhancement of anticancer activity by silibinin and paclitaxel combination on the ovarian cancer. Artificial Cells, Nanomedicine and Biotechnology. 2018 Nov;46(7):1483-1487.
- Momeny M, Ghasemi R et al. Effects of silibinin on growth and invasive properties of human ovarian carcinoma cells through suppression of heregulin/HER3 pathway. Tumour Biol. 2016 Mar;37(3):3913-23; Fan L, Ma Y, Liu Y, Zheng D, Huang G. Silymarin induces cell cycle arrest and apoptosis in ovarian cancer cells. European Journal of Pharmacology. 2014 Nov 15;743:79-88.
- Scambia G, De Vincenzo R et al. Antiproliferative effect of silybin on gynaecological malignancies: synergism with cisplatin and doxorubicin. European Journal of Cancer. 1996 May;32A(5):877-82.
- Amawi H, Hussein NA et al. HM015k, a novel silybin derivative, multi-targets metastatic ovarian cancer cells and is safe in zebrafish toxicity studies. Frontiers in Pharmacology. 2017 Aug 2;8:498.
- Horsman MR, Brown JM et al. Mechanism of action of the selective tumor radiosensitizer nicotinamide. International Journal of Radiation Oncology, Biology, Physics. 1988 Sep;15(3):685-90.
- Horsman MR, Siemann DW, Chaplin DJ, Overgaard J. Nicotinamide as a radiosensitizer in tumours and normal tissues: the importance of drug dose and timing. Radiotherapy and Oncology. 1997 Nov;45(2):167-74.
- Liu Y, Gong W et al. Quercetin induces protective autophagy and apoptosis through ER stress via the p-STAT3/Bcl-2 axis in ovarian cancer. Apoptosis. 2017 Apr;22(4):544-557; Hashemzaei M, Delarami Far A et al. Anticancer and apoptosis‑inducing effects of quercetin in vitro and in vivo. Oncology Reports. 2017 Aug;38(2):819-828.
- Parvaresh A, Razavi R et al. Quercetin and ovarian cancer: an evaluation based on a systematic review. Journal of Research in Medical Sciences. 2016 May 9;21:34. eCollection 2016.
- Shen F, Herenyiova M, Weber G. Synergistic down-regulation of signal transduction and cytotoxicity by tiazofurin and quercetin in human ovarian carcinoma cells. Life Sciences. 1999;64(21):1869-76.
- Chen SS, Michael A, Butler-Manuel SA. Advances in the treatment of ovarian cancer: a potential role of antiinflammatory phytochemicals. Discovery Medicine. 2012 Jan;13(68):7-17.
- Frenkel GD, Caffrey PB. A prevention strategy for circumventing drug resistance in cancer chemotherapy. Current Pharmaceutical Design. 2001 Nov;7(16):1595-614.
- Evans SO, Khairuddin PF, Jameson MB. Optimising selenium for modulation of cancer treatments..Anticancer Research. 2017 Dec;37(12):6497-6509.
- Kim HS, Kim MK et al. Effect of red ginseng on genotoxicity and health-related quality of life after adjuvant chemotherapy in patients with epithelial ovarian cancer: a randomized, double blind, placebo-controlled trial. Nutrients. 2017 Jul 19;9(7). pii: E772.
- Jeffreys M, Redaniel MT, Martin RM. The effect of pre-diagnostic vitamin D supplementation on cancer survival in women: a cohort study within the UK Clinical Practice Research Datalink. BMC Cancer. 2015 Oct 12;15:670.
- Hefner J, Csef H et al. The clinical relevance of beta blockers in ovarian carcinoma: a systematic review. Geburtshilfe und Frauenheilkunde. 2016 Oct;76(10):1050-1056.
- Kobayashi M, Wood PA, Hrushesky WJ. Circadian chemotherapy for gynecological and genitourinary cancers. Chronobiology International. 2002 Jan;19(1):237-51.
- Kumar S, Meuter A et al. Metformin intake is associated with better survival in ovarian cancer: a case-control study. Cancer. 2013;119:555–562.
- Currie CJ, Poole CD et al. Mortality after incident cancer in people with and without type 2 diabetes: impact of metformin on survival. Diabetes Care. 2012;35(2):299-304.
- Lengyel E, Litchfield LM et al. Metformin inhibits ovarian cancer growth and increases sensitivity to paclitaxel in mouse models. American Journal of Obstetrics and Gynecology. 2015 Apr;212(4):479.e1-479.e10.
- Hijaz M, Chhina J et al. Preclinical evaluation of olaparib and metformin combination in BRCA1 wildtype ovarian cancer. Gynecologic Oncology. 2016 Aug;142(2):323-31.
- Mert I, Chhina J et al. Synergistic effect of MEK inhibitor and metformin combination in low grade serous ovarian cancer. Gynecologic Oncology. 2017 Aug;146(2):319-326.
- Chen HH, Chen WC et al. Targeting drug transport mechanisms for improving platinum-based cancer chemotherapy. Expert Opinion on Therapeutic Targets. 2015;19(10):1307-17; Chen HH, Kuo MT. Overcoming platinum drug resistance with copper-lowering agents. Anticancer Research. 2013 Oct;33(10):4157-61.
- Ishida S, McCormick F, Smith-McCune K, Hanahan D. Enhancing tumor-specific uptake of the anticancer drug cisplatin with a copper chelator. Cancer Cell. 2010 Jun 15;17(6):574-83.
- Kim KK, Lange TS, Singh RK, Brard L, Moore RG. Tetrathiomolybdate sensitizes ovarian cancer cells to anticancer drugs doxorubicin, fenretinide, 5-fluorouracil and mitomycin C. BMC Cancer. 2012 Apr 13;12:147.
- Verdoodt F, Dehlendorff C, Friis S, Kjaer SK. Non-aspirin NSAID use and ovarian cancer mortality. Gynecologic Oncology. 2018 Aug;150(2):331-337.
- Merritt MA, Rice MS et al. Pre-diagnosis and post-diagnosis use of common analgesics and ovarian cancer prognosis (NHS/NHSII): a cohort study. Lancet Oncology. 2018 Aug;19(8):1107-1116.
- Pantziarka P, Sukhatme V, Bouche G, Meheus L, Sukhatme VP. Repurposing Drugs in Oncology (ReDO)-diclofenac as an anti-cancer agent. Ecancermedicalscience. 2016;10:610.
- Verdoodt F, Kjaer SK, Friis S. Influence of aspirin and non-aspirin NSAID use on ovarian and endometrial cancer: summary of epidemiologic evidence of cancer risk and prognosis. Maturitas. 2017 Jun;100:1-7.
- Huang Y, Lichtenberger LM et al. Antitumor and antiangiogenic effects of aspirin-PC in ovarian cancer. Molecular Cancer Therapeutics. 2016 Dec;15(12):2894-2904.
- Pantziarka P, Sukhatme V, Bouche G, Meheus L, Sukhatme VP. Repurposing Drugs in Oncology (ReDO)-diclofenac as an anti-cancer agent. Ecancermedicalscience. 2016;10:610.
- Khan MS, Fatima K, Rameez. Impact of statins on risk and survival of ovarian cancer. Journal of Gynecologic Oncology. 2015 Jul;26(3):240-1; Urpilainen E, Marttila M et al. Prognosis of ovarian cancer in women with type 2 diabetes using metformin and other forms of antidiabetic medication or statins: a retrospective cohort study. BMC Cancer. 2018 Jul 28;18(1):767; Verdoodt F, Kjaer Hansen M et al. Statin use and mortality among ovarian cancer patients: a population-based cohort study. International Journal of Cancer. 2017 Jul 15;141(2):279-286.
- Li B, Li X et al. Dichloroacetate and metformin synergistically suppress the growth of ovarian cancer cells. Oncotarget. 2016 Sep 13;7(37):59458-59470.
- Xintaropoulou C, Ward C et al. A comparative analysis of inhibitors of the glycolysis pathway in breast and ovarian cancer cell line models. Oncotarget. 2015 Sep 22;6(28):25677-95; Saed GM, Fletcher NM, Jiang ZL, Abu-Soud HM, Diamond MP. Dichloroacetate induces apoptosis of epithelial ovarian cancer cells through a mechanism involving modulation of oxidative stress. Reproductive Sciences. 2011 Dec;18(12):1253-61.
- Zhang Y, Guo G et al. A hybrid platinum drug dichloroacetate-platinum(II) overcomes cisplatin drug resistance through dual organelle targeting. Anticancer Drugs. 2015 Aug;26(7):698-705.
- Olszewski U, Poulsen TT et al. In vitro cytotoxicity of combinations of dichloroacetate with anticancer platinum compounds. Clinical Pharmacology. 2010;2:177-83.
- Donahue RN, McLaughlin PJ, Zagon IS. The opioid growth factor (OGF) and low dose naltrexone (LDN) suppress human ovarian cancer progression in mice. Gynecologic Oncology. 2011 Aug;122(2):382-8.
- Donahue RN, McLaughlin PJ, Zagon IS. Low-dose naltrexone suppresses ovarian cancer and exhibits enhanced inhibition in combination with cisplatin. Experimental Biology and Medicine (Maywood). 2011 Jul;236(7):883-95.
- Tomar V, Kukreti S, Prakash S, Madan J, Chandra R. Noscapine and its analogs as chemotherapeutic agent: current updates. Current Topics in Medicinal Chemistry. 2017;17(2):174-188.
- Zhou J, Gupta K et al. Paclitaxel-resistant human ovarian cancer cells undergo c-Jun NH2-terminal kinase-mediated apoptosis in response to noscapine. Journal of Biological Chemistry. 2002 Oct 18;277(42):39777-85.
- Shen W, Liang B, Yin J, Li X, Cheng J. Noscapine increases the sensitivity of drug-resistant ovarian cancer cell line SKOV3/DDP to cisplatin by regulating cell cycle and activating apoptotic pathways. Cell Biochemistry and Biophysics. 2015 May;72(1):203-13; Su W, Huang L et al. Noscapine sensitizes chemoresistant ovarian cancer cells to cisplatin through inhibition of HIF-1α. Cancer Letters. 2011 Jun 1;305(1):94-9.
- Martin LTP, Nachtigal MW et al. Bitter taste receptors are expressed in human epithelial ovarian and prostate cancers cells and noscapine stimulation impacts cell survival. Molecular and Cellular Biochemistry. 2018 Oct 22.
- Li Y, Zhou YF et al. Chinese expert consensus on cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal malignancies. World Journal of Gastroenterology. 2016 Aug 14;22(30):6906-16.
- Jewell A, McMahon M, Khabele D. Heated intraperitoneal chemotherapy in the management of advanced ovarian cancer. Cancers (Basel). 2018 Sep 1;10(9). pii: E296; van Driel WJ, Koole SN, Sonke GS. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. New England Journal of Medicine. 2018 Apr 5;378(14):1363-1364; Hotouras A, Desai D et al. Heated intraperitoneal chemotherapy (HIPEC) for patients with recurrent ovarian cancer: a systematic literature review. International Journal of Gynecological Cancer. 2016 May;26(4):661-70; Kireeva GS, Gafton GI et al. HIPEC in patients with primary advanced ovarian cancer: Is there a role? A systematic review of short- and long-term outcomes. Surgical Oncology. 2018 Jun;27(2):251-258; Chua TC, Robertson G et al. Intraoperative hyperthermic intraperitoneal chemotherapy after cytoreductive surgery in ovarian cancer peritoneal carcinomatosis: systematic review of current results. Journal of Cancer Research and Clinical Oncology. 2009 Dec;135(12):1637-45; Huo YR, Richards A, Liauw W, Morris DL. Hyperthermic intraperitoneal chemotherapy (HIPEC) and cytoreductive surgery (CRS) in ovarian cancer: a systematic review and meta-analysis. European Journal of Surgical Oncology. 2015 Dec;41(12):1578-89; Helm CW, Richard SD et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer: first report of the HYPER-O registry. International Journal of Gynecological Cancer. 2010 Jan;20(1):61-9; Di Giorgio A, Naticchioni E et al. Cytoreductive surgery (peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of diffuse peritoneal carcinomatosis from ovarian cancer. Cancer. 2008 Jul 15;113(2):315-25; Ryu KS, Kim JH et al. Effects of intraperitoneal hyperthermic chemotherapy in ovarian cancer. Gynecologic Oncology. 2004 Aug;94(2):325-32.
- Polom K, Roviello G et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for treatment of ovarian cancer. International Journal of Hyperthermia. 2016 May;32(3):298-310; Cascales-Campos P, Gil J, Feliciangeli E, Parrilla P. HIPEC in ovarian cancer: treatment of a new era or is it the end of the pipeline? Gynecologic Oncology. 2015 Nov;139(2):363-8.
- Kleef R, Kekic S, Ludwig N. Successful treatment of advanced ovarian cancer with thermochemotherapy and adjuvant immune therapy. Case Reports in Oncology. 2012 May;5(2):212-5; Douwes F, BogoviC J, Douwes O, Migeod F, Grote C. Whole-body hyperthermia in combination with platinum-containing drugs in patients with recurrent ovarian cancer. International Journal of Clinical Oncology. 2004 Apr;9(2):85-91; Atmaca A, Al-Batran SE et al. Whole-body hyperthermia (WBH) in combination with carboplatin in patients with recurrent ovarian cancer—a phase II study. Gynecologic Oncology. 2009 Feb;112(2):384-8; Westermann AM, Grosen EA et al. A pilot study of whole body hyperthermia and carboplatin in platinum-resistant ovarian cancer. European Journal of Cancer. 2001 Jun;37(9):1111-7; Robins HI, Cohen JD, Schmitt CL Phase I clinical trial of carboplatin and 41.8 degrees C whole-body hyperthermia in cancer patients. Journal of Clinical Oncology. 1993 Sep;11(9):1787-94; Cohen JD, Robins HI. Whole body hyperthermia and intraperitoneal carboplatin in residual ovarian cancer. Advances in Experimental Medicine and Biology. 1990;267:197-202; Robins HI, Longo WL et al. Phase I trial of lonidamine with whole body hyperthermia in advanced cancer. Cancer Research. 1988 Nov 15;48(22):6587-92.
- Lemanne D, Maizes V. Advising women undergoing treatment for breast cancer: a narrative review. Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):902-909; Lindau ST, Abramsohn EM et al. Physical examination of the female cancer patient with sexual concerns: what oncologists and patients should expect from consultation with a specialist. CA: a Cancer Journal for Clinicians. 2016 May;66(3):241-63.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10): 882.
- Ben-Ayre E, Samuels N, Lavie O. Integrative medicine for female patients with gynecologic cancer. The Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10): 882.
- Macciò A, Madeddu C et al. A randomized phase III clinical trial of a combined treatment for cachexia in patients with gynecological cancers: evaluating the impact on metabolic and inflammatory profiles and quality of life. Gynecologic Oncology. 2012 Mar;124(3):417-25.
- Pulsed low-dose pelvic reirradiation safe, provided tangible benefit for patients with few other options. Fox Chase Cancer Center, September 22, 2020. Viewed September 30, 2020; Paly JJ, Deng M et al. Pelvic reirradiation utilizing pulsed low-dose rate radiation therapy. American Journal of Clinical Oncology. 2020 Oct;43(10):748-751.
- Panahi Y, Saadat A, Beiraghdar F, Sahebkar A. Adjuvant therapy with bioavailability-boosted curcuminoids suppresses systemic inflammation and improves quality of life in patients with solid tumors: a randomized double-blind placebo-controlled trial. Phytotherapy Research. 2014 Oct;28(10):1461-7.
- Marx W, Ried K et al. Ginger—mechanism of action in chemotherapy-induced nausea and vomiting: a review. Critical Reviews in Food Science and Nutrition. 2017 Jan 2;57(1):141-146; Sheikhi MA, Ebadi A, Talaeizadeh A, Rahmani H. Alternative methods to treat nausea and v—omiting from cancer chemotherapy. Chemotherapy Research and Practice. 2015;2015:818759; Marx W, Kiss N, Isenring L. Is ginger beneficial for nausea and vomiting? An update of the literature. Current Opinion in Supportive and Palliative Care. 2015 Jun;9(2):189-95; Marx WM, Teleni L et al. Ginger (Zingiber officinale) and chemotherapy-induced nausea and vomiting: a systematic literature review. Nutrition Reviews. 2013 Apr;71(4):245-54; Lee J, Oh H. Ginger as an antiemetic modality for chemotherapy-induced nausea and vomiting: a systematic review and meta-analysis. Oncology Nursing Forum. 2013 Mar;40(2):163-70.
- Sontakke S, Thawani V, Naik MS. Ginger as an antiemetic in nausea and vomiting induced by chemotherapy: a randomized, cross-over, double blind study. Indian Journal of Pharmacology. 2003;35(1):32–36.
- Sanaati F, Najafi S, Kashaninia Z, Sadeghi M. Effect of ginger and chamomile on nausea and vomiting caused by chemotherapy in Iranian women with breast cancer. Asian Pacific Journal of Cancer Prevention. 2016;17(8):4125-9; Arslan M, Ozdemir L. Oral intake of ginger for chemotherapy-induced nausea and vomiting among women with breast cancer. Clinical Journal of Oncology Nursing. 2015 Oct;19(5):E92-7.
- Kim HS, Kim MK et al. Effect of red ginseng on genotoxicity and health-related quality of life after adjuvant chemotherapy in patients with epithelial ovarian cancer: a randomized, double blind, placebo-controlled trial. Nutrients. 2017 Jul 19;9(7). pii: E772.
- Yennurajalingam S, Tannir NM et al. A double-blind, randomized, placebo-controlled trial of Panax ginseng for cancer-related fatigue in patients with advanced cancer. Journal of the National Comprehensive Cancer Network. 2017 Sep;15(9):1111-1120.
- Arring NM, Millstine D, Marks LA, Nail LM. Ginseng as a treatment for fatigue: a systematic review. Journal of Alternative and Complementary Medicine. 2018 Jul;24(7):624-633.
- Chen MH, May BH, Zhou IW, Zhang AL, Xue CC. Integrative medicine for relief of nausea and vomiting in the treatment of colorectal cancer using oxaliplatin-based chemotherapy: a systematic review and meta-analysis. Phytotherapy Research. 2016 May;30(5):741-53.
- Brami C, Bao T, Deng G. Natural products and complementary therapies for chemotherapy-induced peripheral neuropathy: a systematic review. Critical Reviews in Oncology/Hematology. 2016 Feb;98:325-34; Mondal S, Choudhury KB, Sharma S, Gupta A, DuttaS. Comparative study among glutamine, acetyl-L-carnitine, vitamin-E and methylcobalamine for treatment of paclitaxel-induced peripheral neuropathy. Clinical Cancer Investigation Journal. 2014;3(3):213-219; Argyriou AA, Chroni E et al. Vitamin E for prophylaxis against chemotherapy-induced neuropathy: a randomized controlled trial. Neurology. 2005 Jan 11;64(1):26-31; Pace A, Savarese A et al. Neuroprotective effect of vitamin E supplementation in patients treated with cisplatin chemotherapy. Journal of Clinical Oncology. 2003 Mar 1;21(5):927-31.
- Abrams DI. The therapeutic effects of cannabis and cannabinoids: an update from the National Academies of Sciences, Engineering and Medicine report. European Journal of Internal Medicine. 2018 Mar;49:7-11.
- Mücke M, Weier M. Systematic review and meta-analysis of cannabinoids in palliative medicine. Journal of Cachexia, Sarcopenia and Muscle. 2018 Feb 5.
- Ahn WS, Kim DJ et al. Natural killer cell activity and quality of life were improved by consumption of a mushroom extract, Agaricus blazei Murill Kyowa, in gynecological cancer patients undergoing chemotherapy. International Journal of Gynecological Cancer. 2004 Jul-Aug;14(4):589-94.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Poole J. Individualised homeopathy after cancer treatment. Nursing Times. 2014 Oct 8-14;110(41):17-9.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Pelzer F, Tröger W, Nat DR. Complementary treatment with mistletoe extracts during chemotherapy: safety, neutropenia, fever, and quality of life assessed in a randomized study. Journal of Alternative and Complementary Medicine. 2018 Sep/Oct;24(9-10):954-961.
- Freuding M, Keinki C et al. Mistletoe in oncological treatment: a systematic review: part 2: quality of life and toxicity of cancer treatment. Journal of Cancer Research and Clinical Oncology. 2019 Jan 23.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Hao J, Zhu X, Bensoussan A. Effects of nonpharmacological interventions in chemotherapy-induced peripheral neuropathy: an overview of systematic reviews and meta-analyses. Integrative Cancer Therapies. Jan-Dec 2020;19:1534735420945027; Noh H, Yoon SW, Park B. A systematic review of herbal medicine for chemotherapy-induced peripheral neuropathy (CIPN). Evidence Based Complementary and Alternative Medicine. 2018 Feb 14;2018:6194184; Wei X, Zhu L, Wang H, Wang C, Deng Q, Li X. Efficacy of traditional Chinese medicines in preventing oxaliplatin-induced peripheral neurotoxicity in cancer patients: a network meta-analysis. Chinese Herb Med. 2017;9(2):161-168; Deng B, Jia L, Cheng Z. Radix astragali-based Chinese herbal medicine for oxaliplatin-induced peripheral neuropathy: a systematic review and meta-analysis. Evidence-based Complementary and Alternative Medicine. 2016;2016:2421876.
- Sieja K, Talerczyk M. Selenium as an element in the treatment of ovarian cancer in women receiving chemotherapy. Gynecologic Oncology. 2004 May;93(2):320-7.
- Dias MA, Sampaio AL, Venosa AR, Meneses Ede A, Oliveira CA. The chemopreventive effect of Ginkgo biloba extract 761 against cisplatin ototoxicity: a pilot study. International Tinnitus Journal. 2015;19(2):12-9; Aydin D, Peker EG et al. Effects of Ginkgo biloba extract on brain oxidative condition after cisplatin exposure. Clinical and Investigative Medicine. 2016 Dec 1;39(6):27511.
- Etheridge AS, Kroll DJ, Mathews JM. Inhibition of paclitaxel metabolism in vitro in human hepatocytes by Ginkgo biloba preparations. Journal of Dietary Supplements. 2009;6(2):104-10.
- Agbabiaka TB, Wider B, Watson LK, Goodman C. Concurrent use of prescription drugs and herbal medicinal products in older adults: a systematic review. Drugs & Aging. 2017 Dec;34(12):891-905.
- Mei N, Guo X et al. Review of Ginkgo biloba-induced toxicity, from experimental studies to human case reports. Journal of Environmental Science and Health. Part C, Environmental Carcinogenisis and Ecotoxicology Reviews. 2017 Jan 2;35(1):1-28.
- Nunes SC, Serpa J. Glutathione in ovarian cancer: a double-edged sword. International Journal of Molecular Sciences. 2018 Jun 26;19(7). pii: E1882; Smyth JF, Bowman A, Perren T et al. Glutathione reduces the toxicity and improves quality of life of women diagnosed with ovarian cancer treated with cisplatin: results of a double-blind, randomised trial. Annals of Oncology. 1997;8(6):569-573.
- Leal AD, Qin R et al. North Central Cancer Treatment Group/Alliance trial N08CA-the use of glutathione for prevention of paclitaxel/carboplatin-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled study. Cancer. 2014 Jun 15;120(12):1890-7.
- Bogliun G, Marzorati L et al. Neurotoxicity of cisplatin +/- reduced glutathione in the first-line treatment of advanced ovarian cancer. International Journal of Gynecological Cancer. 1996;6:415-419.
- Colombo N, Bini S. et al. Weekly cisplatin and glutathione in relapsed ovarian carcinoma. International Journal of Gynecological Cancer. 1995;5:81-86.
- Ma Y, Chapman J et al. High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Science Translational Medicine. 2014 Feb 5;6(222):222ra18.
- Loven D, Levavi H et al. Long-term glutamate supplementation failed to protect against peripheral neurotoxicity of paclitaxel. European Journal of Cancer Care (Engl). 2009 Jan;18(1):78-83.
- Kim HS, Kim MK et al. Effect of red ginseng on genotoxicity and health-related quality of life after adjuvant chemotherapy in patients with epithelial ovarian cancer: a randomized, double blind, placebo-controlled trial. Nutrients. 2017 Jul 19;9(7). pii: E772.
- Sieja K, Talerczyk M. Selenium as an element in the treatment of ovarian cancer in women receiving chemotherapy. Gynecologic Oncology. 2004 May;93(2):320-7.
- Muecke R, Micke O et al. Impact of treatment planning target volumen (PTV) size on radiation induced diarrhoea following selenium supplementation in gynecologic radiation oncology--a subgroup analysis of a multicenter, phase III trial. Radiation Oncology. 2013 Mar 25;8:72.
- Muecke R, Micke O et al. Selenium in radiation oncology—15 years of experiences in Germany. Nutrients. 2018 Apr 13;10(4). pii: E483.
- Sánchez-González PD, López-Hernández FJ et al. Differential effect of quercetin on cisplatin-induced toxicity in kidney and tumor tissues. Food and Chemical Toxicology. 2017 Sep;107(Pt A):226-236.
- Rezk YA, Balulad SS, Keller RS, Bennett JA. Use of resveratrol to improve the effectiveness of cisplatin and doxorubicin: study in human gynecologic cancer cell lines and in rodent heart. American Journal of Obstetrics and Gynecology. 2006 May;194(5):e23-6.
- Donahue RN, McLaughlin PJ, Zagon IS. Low-dose naltrexone suppresses ovarian cancer and exhibits enhanced inhibition in combination with cisplatin. Experimental Biology and Medicine (Maywood). 2011 Jul;236(7):883-95.
- Mao-Ying QL, Kavelaars A et al. The anti-diabetic drug metformin protects against chemotherapy-induced peripheral neuropathy in a mouse model. PLoS One. 2014 Jun 23;9(6):e10070; Zhou W, Kavelaars A, Heijnen CJ. Metformin prevents cisplatin-induced cognitive impairment and brain damage in mice. PLoS One. 2016 Mar 28;11(3):e0151890.
- Zhou W, Kavelaars A, Heijnen CJ. Metformin prevents cisplatin-induced cognitive impairment and brain damage in mice. PLoS One. 2016 Mar 28;11(3):e0151890.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecol Oncol. 2011 Nov;123(2):346-50.
- Bober SL, Recklitis CJ, Michaud AL, Wright AA. Improvement in sexual function after ovarian cancer: effects of sexual therapy and rehabilitation after treatment for ovarian cancer. Cancer. 2018 Jan 1;124(1):176-182.
- Petersen RW, Quinlivan JA. Preventing anxiety and depression in gynaecological cancer: a randomised controlled trial.BJOG. 2002 Apr;109(4):386-94.
- Goerling U, Jaeger C et al. The efficacy of short-term psycho-oncological interventions for women with gynaecological cancer: a randomized study. Oncology. 2014;87(2):114-24.
- Spiegel D. The use of hypnosis in controlling cancer pain. CA: A Cancer Journal for Clinicians. 1985 Jul-Aug;35(4):221-31.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Danhauer SC, Tooze JA et al. Restorative yoga for women with ovarian or breast cancer: findings from a pilot study. Journal of the Society for Integrative Oncology. 2008 Spring;6(2):47-58.
- Lu W, Matulonis UA et al. The feasibility and effects of acupuncture on quality of life scores during chemotherapy in ovarian cancer: results from a pilot, randomized sham-controlled trial. Medical Acupuncture. 2012 Dec;24(4):233-240.
- Rithirangsriroj K, Manchana T, Akkayagorn L. Efficacy of acupuncture in prevention of delayed chemotherapy induced nausea and vomiting in gynecologic cancer patients. Gynecologic Oncology. 2015 Jan;136(1):82-6.
- Liu YQ, Sun S et al. Wrist-ankle acupuncture and ginger moxibustion for preventing gastrointestinal reactions to chemotherapy: a randomized controlled trial. Chinese Journal of Integrative Medicine. 2015 Sep;21(9):697-702.
- Paice JA, Portenoy R et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology. 2016 Sep 20;34(27):3325-45.
- CancerNet. Peripheral Neuropathy. American Society of Clinical Oncology. May 2017. Viewed March 14, 2018.
- Gross AH, Cromwell J, Fonteyn M, Matulonis UA, Hayman LL. Hopelessness and complementary therapy use in patients with ovarian cancer. Cancer Nursing. 2013 Jul-Aug;36(4):256-64.
- Donoyama N, Satoh T, Hamano T, Ohkoshi N, Onuki M. Physical effects of Anma therapy (Japanese massage) for gynecologic cancer survivors: a randomized controlled trial. Gynecologic Oncology. 2016 Sep;142(3):531-8.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Greenlee H, DuPont-Reyes MJ et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA A Cancer Journal for Clinicians. 2017 May 6;67(3):194-232.
- Bauersfeld SP, Kessler CS et al. The effects of short-term fasting on quality of life and tolerance to chemotherapy in patients with breast and ovarian cancer: a randomized cross-over pilot study. BMC Cancer. 2018 Apr 27;18(1):476.
- Riedinger C, Kimball KJ et al. Water-only fasting and its effect on chemotherapy administration in gynecologic malignancies. Society of Gynecologic Oncology 20/20 Annual Meeting on Women's Cancer.
- Safdie FM, Dorff T et al. Fasting and cancer treatment in humans: a case series report. Aging (Milano) 2009;1:988–1007.
- Hisada Y, Mackman N. Cancer-associated pathways and biomarkers of venous thrombosis. Blood. 2017 Sep 28;130(13):1499-1506.
- Block KI. Life over Cancer: The Block Center Program for Integrative Cancer Treatment. New York: Bantam Dell. 2009. p. 368-390.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013; Dixon-Suen SC, Nagle CM et al. Adult height is associated with increased risk of ovarian cancer: a Mendelian randomisation study. British Journal of Cancer. 2018 Apr;118(8):1123-1129.
- Continuous Update Project. Ovarian cancer: how diet, nutrition and physical activity affect ovarian cancer risk. Diet and Cancer Report. World Cancer Research Fund International. Viewed January 31, 2019; Turck D; Comité de nutrition de la Société française de pédiatrie; Breast feeding: health benefits for child and mother]. [Article in French] Archives de Pediatrie. 2005 Dec;12 Suppl 3:S145-65; Foong KW, Bolton H. Obesity and ovarian cancer risk: a systematic review. Post Reproductive Health. 2017 Dec;23(4):183-198; La Vecchia C. Ovarian cancer: epidemiology and risk factors. European Journal of Cancer and Prevention. 2017 Jan;26(1):55-62; Harris HR, Rice MS et al. Lifestyle and reproductive factors and ovarian cancer risk by p53 and MAPK expression. Cancer Epidemiology, Biomarkers & Prevention. 2018 Jan;27(1):96-102.
- Dun A, Zhao X et al. Association between night-shift work and cancer risk: updated systematic review and meta-analysis. Frontiers in Oncology. 2020 Jun 23;10:1006.
- Carter BD, Diver WR, Hildebrand JS, Patel AV, Gapstur SM. Circadian disruption and fatal ovarian cancer. American Journal of Preventive Medicine. 2014 Mar;46(3 Suppl 1):S34-41; Poole EM, Schernhammer ES, Tworoger SS. Rotating night shift work and risk of ovarian cancer. Cancer Epidemiology, Biomarkers & Prevention. 2011 May;20(5):934-8.
- Nené NR, Reisel D et al. Association between the cervicovaginal microbiome, BRCA1 mutation status, and risk of ovarian cancer: a case-control study. Lancet Oncology. 2019 Aug;20(8):1171-1182.
- ASCO Post Staff. Study clarifies time-dependent effects of oral contraceptives on risk of ovarian, endometrial, and breast cancers. ASCO Post. December 23, 2020. Viewed January 5, 2021; Karlsson T, Johansson T, Höglund J, Ek WE, Johansson Å. Time-dependent effects of oral contraceptive use on breast, ovarian and endometrial cancers. Cancer Research. 2020 Dec 17:canres.2476.2020.
- Qu XL, Fang Y, Zhang M, Zhang YZ. Phytoestrogen intake and risk of ovarian cancer: a meta- analysis of 10 observational studies. Asian Pacific Journal of Cancer Prevention. 2014;15(21):9085-91; Bandera EV, King M et al. Phytoestrogen consumption from foods and supplements and epithelial ovarian cancer risk: a population-based case control study. BMC Womens Health. 2011 Sep 23;11:40..
- Sahin K, Yenice E et al. Genistein prevents development of spontaneous ovarian cancer and inhibits tumor growth in hen model. Cancer Prevention and Research (Philadelphia, PA). 2019 Jan 16.
- Terry PD, Qin B et al. Supplemental selenium may decrease ovarian cancer risk in African-American women. Journal of Nutrition. 2017 Apr;147(4):621-627.
- Fleischauer AT, Olson SH et al. Dietary antioxidants, supplements, and risk of epithelial ovarian cancer. Nutrition and Cancer. 2001;40(2):92-8.
- Thomson CA, Neuhouser ML et al. The role of antioxidants and vitamin A in ovarian cancer: results from the Women's Health Initiative. Nutrition and Cancer. 2008;60(6):710-9; Fairfield KM, Hankinson SE et al. Risk of ovarian carcinoma and consumption of vitamins A, C, and E and specific carotenoids: a prospective analysis. Cancer. 2001 Nov 1;92(9):2318-26.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- Raymond YC, Glenda CS, Meng LK. Effects of high doses of vitamin C on cancer patients in Singapore: nine cases. Integrative Cancer Therapies. 2016;15(2):197-204.
- Drisko JA, Chapman J, Hunter VJ. The use of antioxidants with first-line chemotherapy in two cases of ovarian cancer. Journal of the American College of Nutrition. 2003 Apr;22(2):118-23.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Ye B, Aponte M et al. Ginkgo biloba and ovarian cancer prevention: epidemiological and biological evidence. Cancer Letters. 2007 Jun 18;251(1):43-52.
- Jiang W, Qiu W et al. Ginkgo may prevent genetic-associated ovarian cancer risk: multiple biomarkers and anticancer pathways induced by ginkgolide B in BRCA1-mutant ovarian epithelial cells. European Journal of Cancer Prevention. 2011 Nov;20(6):508-17.
- Agbabiaka TB, Wider B, Watson LK, Goodman C. Concurrent use of prescription drugs and herbal medicinal products in older adults: a systematic review. Drugs & Aging. 2017 Dec;34(12):891-905.
- Mei N, Guo X et al. Review of Ginkgo biloba-induced toxicity, from experimental studies to human case reports. Journal of Environmental Science and Health. Part C, Environmental Carcinogenisis and Ecotoxicology Reviews. 2017 Jan 2;35(1):1-28.
- Dikshit A, Hales K, Hales DB. Whole flaxseed diet alters estrogen metabolism to promote 2-methoxtestradiol-induced apoptosis in hen ovarian cancer. Journal of Nutritional Biochemistry. 2017 Apr;42:117-125.
- Sahin K, Yenice E et al. Lycopene protects against spontaneous ovarian cancer formation in laying hens. Journal of Cancer Prevention. 2018 Mar;23(1):25-36.
- Koushik A, Wang M et al. Intake of vitamins A, C, and E and folate and the risk of ovarian cancer in a pooled analysis of 10 cohort studies. Cancer Causes & Control. 2015 Sep;26(9):1315-27.
- Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA. Dietary intake and ovariancancer risk: a systematic review. Cancer Epidemiology, Biomarkers & Prevention.
- 2014 Feb;23(2):255-73.
- Qin B, Moorman PG et al. Dairy, calcium, vitamin D and ovarian cancer risk in African-American women. British Journal Cancer. 2016 Oct 25;115(9):1122-1130.
- Verdoodt F, Kjaer SK, Friis S. Influence of aspirin and non-aspirin NSAID use on ovarian and endometrial cancer: summary of epidemiologic evidence of cancer risk and prognosis. Maturitas. 2017 Jun;100:1-7; Zhang D, Bai B, Xi Y, Wang T, Zhao Y. Is aspirin use associated with a decreased risk of ovarian cancer? A systematic review and meta-analysis of observational studies with dose-response analysis. Gynecologic Oncology. 2016 Aug;142(2):368-77; Baandrup L, Faber MT et al. Nonsteroidal anti-inflammatory drugs and risk of ovarian cancer: systematic review and meta-analysis of observational studies. Acta Obstetricia et Gynecologica Scandinavica. 2013 Mar;92(3):245-55.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Khan MS, Fatima K, Rameez. Impact of statins on risk and survival of ovarian cancer. Journal of Gynecologic Oncology. 2015 Jul;26(3):240-1.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Panahi Y, Saadat A, Beiraghdar F, Sahebkar A. Adjuvant therapy with bioavailability-boosted curcuminoids suppresses systemic inflammation and improves quality of life in patients with solid tumors: a randomized double-blind placebo-controlled trial. Phytotherapy Research. 2014 Oct;28(10):1461-7.
- Ferguson LR, Chen H et al. Genomic instability in human cancer: molecular insights and opportunities for therapeutic attack and prevention through diet and nutrition. Seminars in Cancer Biology. 2015 Dec;35 Suppl:S5-S24.
- Chobotova K, Vernallis AB, Majid FA.Bromelain's activity and potential as an anti-cancer agent: current evidence and perspectives. Cancer Letters. 2010 Apr 28;290(2):148-56.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Chen X, Anderson JJ. Isoflavones inhibit proliferation of ovarian cancer cells in vitro via an estrogen receptor-dependent pathway. Nutrition and Cancer. 2001;41(1-2):165-71; Liu J, Viswanadhapalli S et al. Therapeutic utility of natural estrogen receptor beta agonists on ovarian cancer. Oncotarget. 2017 Jul 25;8(30):50002-50014.
- Alschuler LN, Gazella KA. The Definitive Guide to Cancer, 3rd Edition: An Integrative Approach to Prevention, Treatment, and Healing. Berkeley, California: Celestial Arts. 2010; Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
- McKinney N. Naturopathic Oncology, 3rd Edition. Victoria, BC, Canada: Liaison Press. 2016.
- Ahn WS, Kim DJ et al. Natural killer cell activity and quality of life were improved by consumption of a mushroom extract, Agaricus blazei Murill Kyowa, in gynecological cancer patients undergoing chemotherapy. International Journal of Gynecological Cancer. 2004 Jul-Aug;14(4):589-94.
- Mukai H, Watanabe T, Ando M, Katsumata N. An alternative medicine, Agaricus blazei, may have induced severe hepatic dysfunction in cancer patients. Japanese Journal of Clinical Oncology. 2006 Dec;36(12):808-10.
- Kikuchi Y, Kizawa I et al. Effects of PSK on interleukin-2 production by peripheral lymphocytes of patients with advanced ovarian carcinoma during chemotherapy. Japanese Journal of Cancer Research. 1988 Jan;79(1):125-30.
- Kikuchi Y, Kizawa I et al. [Effects of cimetidine and PSK on interleukin-2 production by PBL in patients with advanced ovarian carcinoma during the course of chemotherapy]. [Article in Japanese] Nihon Sanka Fujinka Gakkai Zasshi. 1987 Nov;39(11):1987-92.
- Ishii K, Kita T et al. [Antitumor effect of PSK and its combined effect with CDDP on ovarian serous adenocarcinoma-bearing nude mice]. [Article in Japanese] Nihon Sanka Fujinka Gakkai Zasshi. 1993 Apr;45(4):333-9.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Lu W, Matulonis UA et al. Acupuncture for chemotherapy-induced neutropenia in patients with gynecologic malignancies: a pilot randomized, sham-controlled clinical trial. Journal of Alternative and Complementary Medicine. 2009 Jul;15(7):745-53.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Judson PL, Dickson EL et al. A prospective, randomized trial of integrative medicine for women with ovarian cancer. Gynecologic Oncology. 2011 Nov;123(2):346-50.
- Alschuler LN, Gazella KA. The Definitive Guide to Thriving after Cancer: A Five-Step Integrative Plan to Reduce the Risk of Recurrence and Build Lifelong Health. Berkeley, California: Ten Speed Press. 2013.
More Information
General Information on Ovarian Cancer Treatments
- National Cancer Institute: Contact Us for Help
Information specialists at the NCI Contact Center are available to help answer your cancer-related questions in English and Spanish whether you are a patient, family member or friend, health care provider, or researcher. We also respond to questions and requests for information about NCI and its programs and provide support in quitting smoking. - American Cancer Society:
- Continuous Update Project. Ovarian cancer: How diet, nutrition and physical activity affect ovarian cancer risk. Diet and Cancer Report. World Cancer Research Fund International.
- Beavis AL, Smith AJ, Fader AN. Lifestyle changes and the risk of developing endometrial and ovarian cancers: opportunities for prevention and management. International Journal of Women’s Health. 2016 May 23;8:151-67.
- McKee D. Off Label Pharmaceutical ‘Cocktails’ For Cancer Treatment (excerpts relevant to ovarian cancer). A4M Integrative Cancer Therapies Module 6. June 6-8, 2013.
- Sweet ES, Standish LJ, Goff BA, Andersen MR. Adverse events associated with complementary and alternative medicine use in ovarian cancer patients. Integrative Cancer Therapies. 2013 Nov;12(6):508-16.
- Kobayashi Y, Banno K, Kunitomi H, Tominaga E, Aoki D. Current state and outlook for drug repositioning anticipated in the field of ovarian cancer. Journal of Gynecologic Oncology. 2019 Jan;30(1):e10.
- Cortez AJ, Tudrej P, Kujawa KA, Lisowska KM. Advances in ovarian cancer therapy. Cancer Chemotherapy and Pharmacology. 2018 Jan;81(1):17-38.
- Halkia E, Spiliotis J. The role of cytoreductive surgery and HIPEC in epithelial ovarian cancer. Journal of BUON. 2015 May;20 Suppl 1:S12-28.
- Moss Report Podcast: Dr. Nasha: Perseverance and Progress
Advocacy and Support Groups
- National Comprehensive Cancer Network: Advocacy and Support Groups; select your topic or cancer of interest from the dropdown menu.
- Other groups not included in above link from National Comprehensive Cancer Network:
- Cancercare: Ovarian Cancer
- Needymeds: Assistance programs for ovarian cancer
- Clearity Foundation: Information and Support
- Moss Report Podcast: Dr. Nasha: Perseverance and Progress
Financial / Support Resources
More from Our Resources Database
- Gurdev Parmar and Tina Kaczor: Textbook of Naturopathic Oncology
- J. Christopher States, Ming Ouyang and C. William Helm: Systems approach to identify environmental exposures contributing to organ-specific carcinogenesis
- Danial E. Baker: Application of chronotherapy to the treatment of cancer: can changing the timing of drug administration influence efficacy and toxicity?
- September 2018 Issue of the Journal of Alternative and Complementary Medicine
- Donald I. Abrams, MD, and Andrew T. Weil, MD: Integrative Oncology, 2nd Edition
- Ralph Moss, PhD: The Moss Reports
Related Pages
Personal Stories
In the News
- Early-stage multi-cancer detection using an extracellular vesicle protein-based blood test
- In mice, a potential new treatment eradicates ovarian and colorectal cancer in days
- Web-based intervention to manage symptoms and quality of life in women with recurrent ovarian cancer
- Measuring financial distress and quality of life over time in patients with gynecologic cancer—making the case to screen early in the treatment course
- FDA approves new imaging drug to help identify ovarian cancer lesions

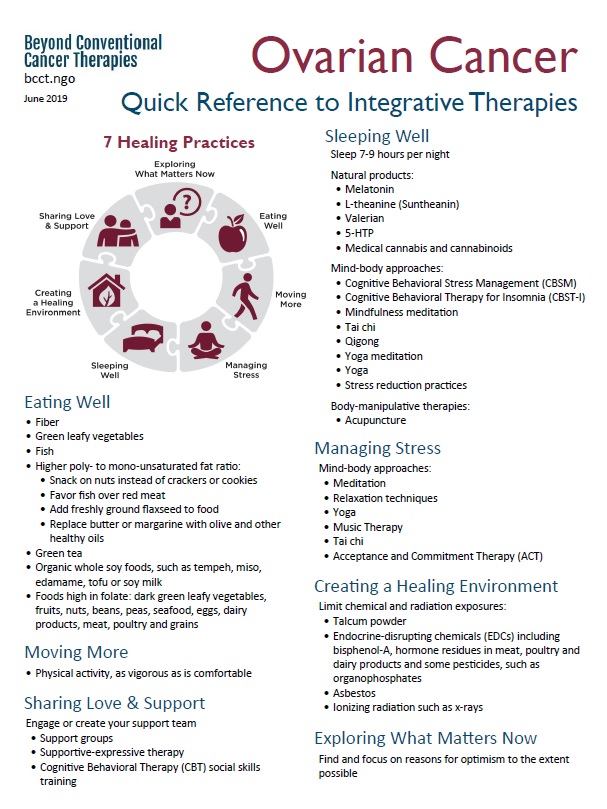

 Nancy Hepp, MS, BCCT Project Manager
Nancy Hepp, MS, BCCT Project Manager